Pelvic floor dysfunction (PFD) is a condition where the muscles, nerves, and connective tissues in the pelvic region fail to function properly. A tight pelvic floor can lead to problems with bladder and bowel control, persistent pelvic pain, and discomfort during daily activities. Though common, many people suffer in silence due to a lack of awareness.
Understanding the intricacies of pelvic floor dysfunction is essential in identifying the problem. For instance, many individuals may not realize that factors such as pregnancy, childbirth, aging, and even high-impact sports can contribute to PFD. In women, the pelvic floor must support additional weight during pregnancy, which can lead to muscle fatigue or damage. Similarly, men may experience pelvic floor issues due to conditions like prostatitis or surgeries that affect the pelvic area.
It’s also important to note that the symptoms of pelvic floor dysfunction can vary widely among individuals. For example, while some may experience urinary urgency, others may have issues with urinary retention. Furthermore, chronic pelvic pain can sometimes be attributed to conditions like endometriosis or interstitial cystitis, highlighting the need for comprehensive evaluation and tailored treatment plans.
PFD can manifest in various ways, including:
Each symptom can have various underlying causes, and understanding these can aid in better management. For instance, pelvic pain during intercourse may not only be due to pelvic floor dysfunction but could also stem from emotional factors, previous trauma, or medical conditions. Therefore, a multidisciplinary approach that includes physical therapy, counseling, and medical intervention is often the most effective way to address these complex issues.
Education about the pelvic floor is equally important. Many individuals remain unaware of how these muscles function and their role in overall health. For example, strengthening exercises, often referred to as Kegel exercises, can be beneficial for both men and women. By learning how to effectively engage and relax these muscles, individuals can improve their symptoms and enhance their quality of life.
If you experience any of these symptoms, seeking professional evaluation is essential. Early intervention can improve your quality of life and prevent further complications. Book a consultation today to find relief.
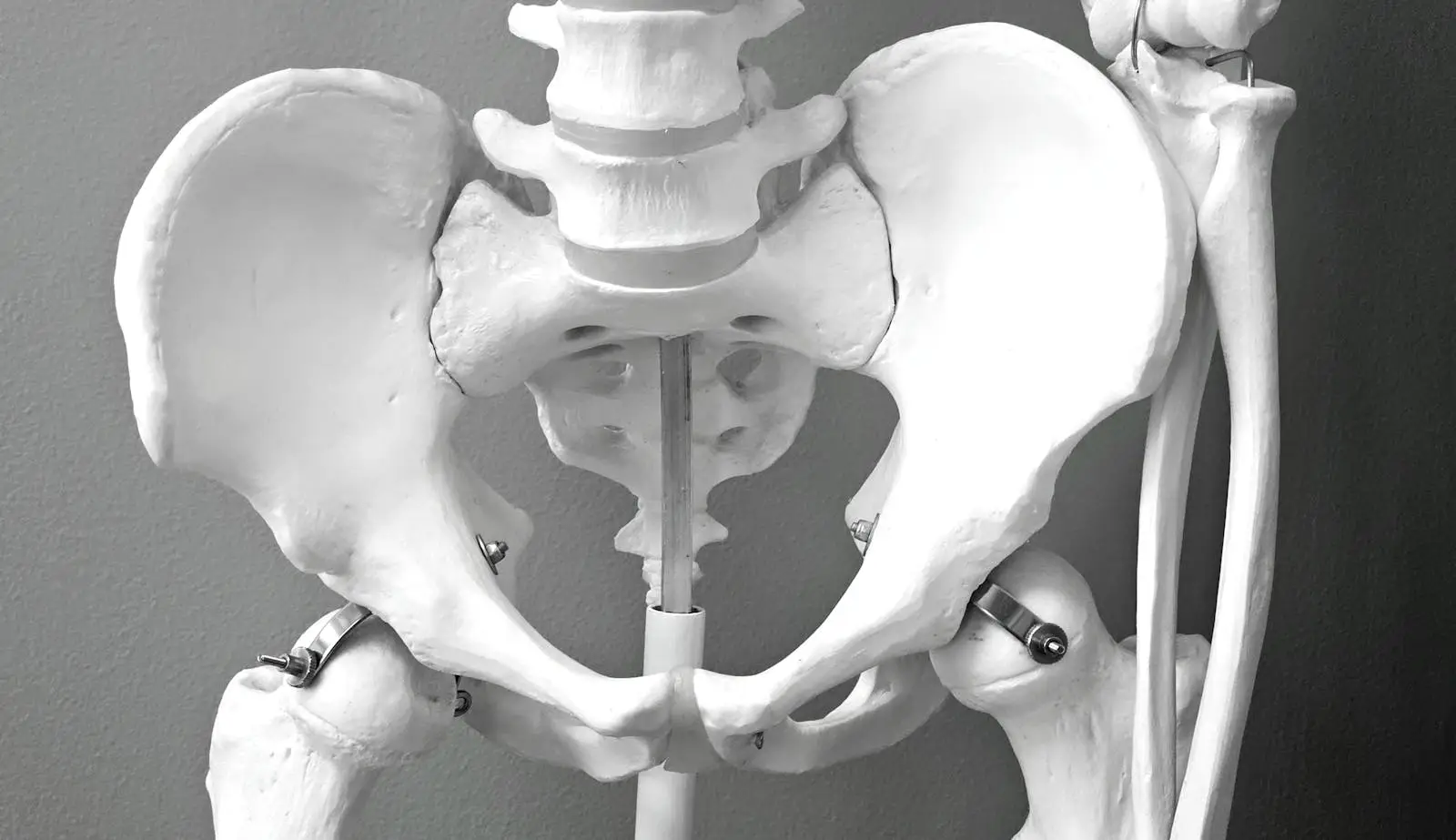
The pelvic floor is a complex network of muscles, nerves, and ligaments that support the bladder, uterus (in women), prostate (in men), and rectum. Dysfunction can result from weakness, tightness, or imbalances in these structures.
When any of these structures are impaired due to injury, muscle imbalances, or chronic tension, symptoms of PFD can arise, leading to discomfort and functional limitations.
Moreover, community support can play a vital role in recovery. Engaging with support groups or online forums allows individuals to share their experiences and coping strategies, reducing feelings of isolation. Many people find comfort in knowing they are not alone in their struggles and can gain insights from others who have successfully navigated similar challenges.
Dry needling is an effective, evidence-based treatment that helps relieve pain, release muscle tension, and restore proper function in the pelvic floor.
This technique can significantly improve symptoms by addressing underlying muscle tightness, nerve irritation, and blood flow issues, leading to better pelvic function and pain relief.
In addition to dry needling, various other therapies exist that can complement pelvic floor rehabilitation. according to the National Institute for Health (NIH) these include biofeedback, which helps patients gain awareness and control over their pelvic floor muscles, and pelvic floor physical therapy, which provides targeted exercises and stretches. Each of these modalities can be tailored to the individual’s specific needs, enhancing overall treatment efficacy.
If pelvic discomfort, urinary issues, or chronic pain are interfering with your daily life, professional treatment can help you regain control. Schedule a consultation with our specialists today and take the first step toward relief.