Persistent “leftover urine” sensation
Feeling unfinished even shortly after voiding, sometimes with repeated attempts to empty that produce only small additional volume.
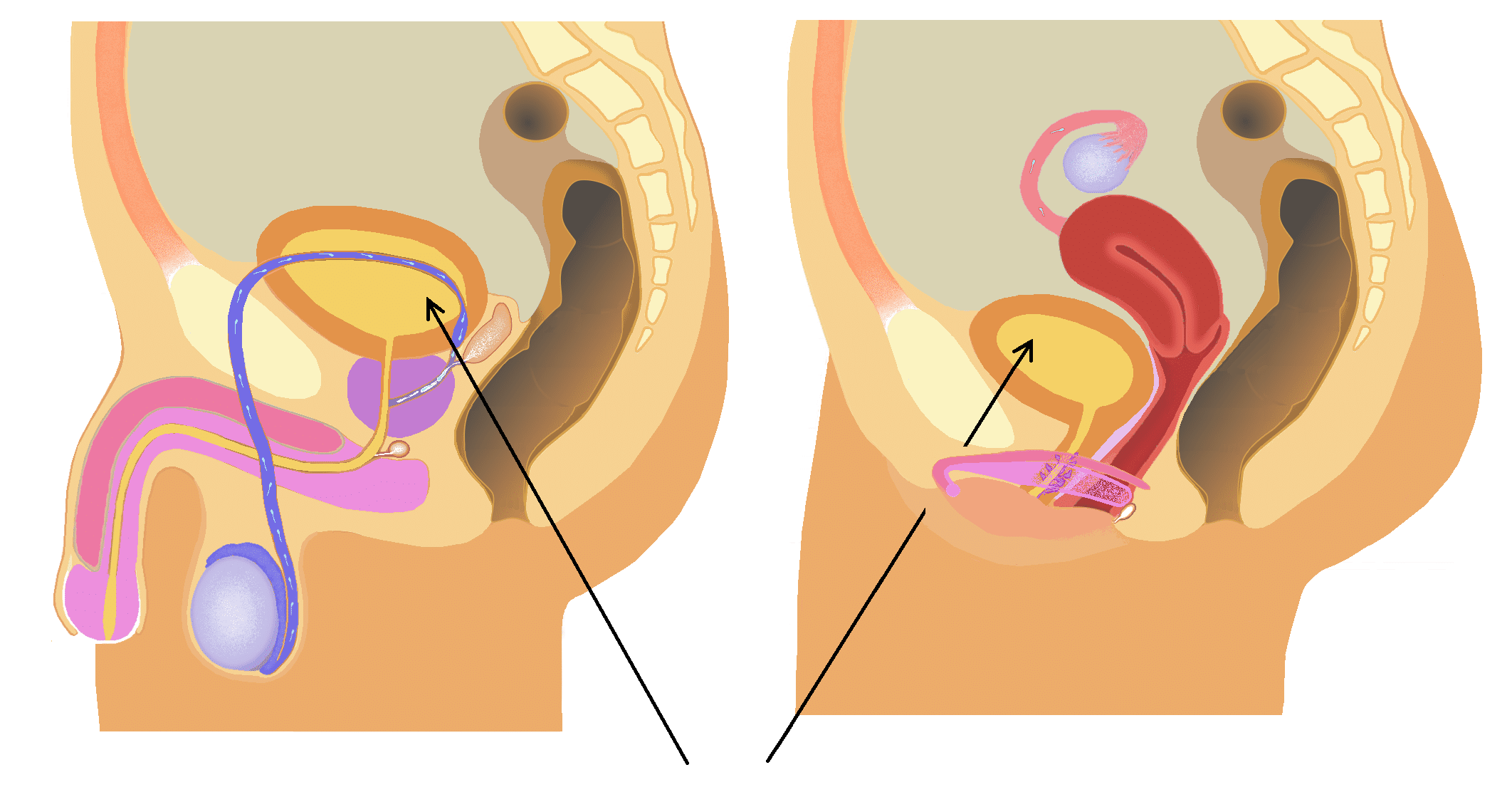
“Incomplete bladder emptying” is a symptom, not a diagnosis. In many cases, the sensation of not emptying is influenced by how the bladder and pelvic floor coordinate. The bladder wall must contract while the pelvic floor and urethral sphincters relax at the right time. If the pelvic floor is guarding, over-recruiting, or poorly timed, the outlet can resist flow, creating a stop-start stream, straining, or a lingering sense of urine left behind.
Incomplete emptying can also be shaped by urgency patterns and nervous system signaling. When the system is sensitized, the brain may interpret bladder sensations as “unfinished” even when volume remaining is small. Other cases involve true retention, which requires medical evaluation to identify causes such as obstruction, medication effects, prostate issues, or neurologic conditions.
Our role in the clinic is to support pelvic floor coordination and comfort, improve tissue tolerance, and reduce guarding and irritability that can contribute to outlet resistance, alongside appropriate medical assessment.
Standard care often focuses on ruling out infection or identifying structural blockage. That is essential, but it can leave a gap when the driver is functional. Imaging and urinalysis do not measure pelvic floor timing, myofascial trigger points that refer urgency, or nerve sensitivity that alters perceived bladder fullness.
Medications may reduce urgency or relax smooth muscle, but they do not consistently retrain pelvic floor release, normalize guarding, or address local myofascial restriction. Procedures can address certain structural problems, yet symptoms may persist if pelvic floor coordination and protective patterns are not evaluated and treated.
Both can be true. Pelvic floor timing and guarding can contribute to incomplete emptying, but new or progressive symptoms should be medically evaluated. We strongly recommend urology assessment if you have measurable retention, recurrent infections, blood in urine, new incontinence, severe pain, fever, or neurologic signs such as leg weakness, numbness in the saddle region, or new bowel changes.
Yes. Standard tests often rule out infection and major structural issues, but they may not assess pelvic floor relaxation timing, myofascial restriction, or nerve sensitivity that can create a strong sensation of incomplete emptying. Our assessment focuses on these functional drivers while encouraging appropriate medical follow-up.
We do not manage acute urinary retention or emergencies. If you cannot urinate, have severe lower abdominal distension, or are told you have significant post-void residual, seek urgent medical care. In stable cases where urology has ruled out urgent causes, we can support pelvic floor coordination and comfort that may contribute to outlet resistance.
Care is assessment-driven and hands-on. Treatment commonly includes acupuncture and dry needling directed at pelvic floor and related hip and abdominal structures to reduce guarding, improve tissue mobility, and support coordinated relaxation. The plan is tailored to your findings and paired with practical strategies for voiding mechanics and flare control.
It varies with symptom duration, irritability, medical factors, and how much guarding is present. Many patients start with a short series of visits to change tone and coordination, then taper as control becomes more consistent. We reassess regularly and adjust based on measurable functional changes like stream consistency and time-to-void.
Possibly. Some medications can affect bladder contraction or sphincter tone, and high training loads can increase pelvic floor guarding through bracing and breath-holding strategies. We review these factors and, when appropriate, recommend discussing medication effects with your prescribing clinician.
While acupuncture does not hurt, you may feel a “de qi” sensation—a deep, dull ache or heaviness at the point of insertion when the thin needles stimulate the connective tissue and nervous system. This is a natural and effective part of the acupuncture treatment, indicating that the acupuncture point is being activated. The patient is always in control, and most find these sensations well-tolerated or enjoyable. Schedule an Appointment or Free Phone Consultation
Most people feel a quick twitch or brief pinch during a dry needling session as the needle interacts with myofascial trigger points or muscle fibers in the affected area, but it’s usually well tolerated and any muscle soreness fades quickly—many patients say the relief is worth it. Schedule an Appointment or Free Phone Consultation
The benefits of dry needling are numerous, especially for pain management. This treatment method effectively targets myofascial trigger points within tight muscles, helping to release muscle tension, improve muscle function and range of motion, and stimulate the body’s natural healing process. It can be particularly effective for soft tissue injuries, overuse injuries, and chronic pain conditions like myofascial pain syndrome by addressing the root causes of discomfort in specific areas of the body. Many find it helps accelerate recovery time from a muscle strain or injury. Schedule an Appointment or Free Phone Consultation
This varies based on the patient’s medical history and condition, but many patients see results over time depending on their condition. Pain-related conditions often initially have quick results, though recovery time can differ. This will be discussed during the initial consultation. Schedule an Appointment or Free Phone Consultation
Yes, acupuncture and dry needling complement most standard medical treatments, including physical therapy treatments or chiropractic care, and Dr. Barber can collaborate with other healthcare providers as needed. Schedule an Appointment or Free Phone Consultation
The first acupuncture appointment or dry needling session includes a detailed initial consultation where Dr. Barber reviews the medical history, discusses specific needs and musculoskeletal condition, performs an assessment, and provides the first personalized treatment option. Schedule an Appointment or Free Phone Consultation
Yes, I treat adults, teens, and children (though I do not specialize in infants or toddlers). I’m experienced in working with sensitive issues and strive to create a welcoming, inclusive space for all patients, including those in the LGBTQIA+ community. For pelvic floor patients who are post-operative following gender-affirming surgery, I do not have specialized training in this area, but if you’re able to provide detailed surgical notes, I’m open to collaborating and finding safe, supportive treatment solutions together. Schedule an Appointment or Free Phone Consultation
Yes — we are an out-of-network provider and can submit to most PPO insurance plans. While we are not contracted with any insurance companies, we want to make it as easy as possible for you to use your benefits when available.
We do not participate with Medicare or Medicaid, including Part C out-of-network coverage.
✔ Claims Submitted on Your Behalf
We now submit out-of-network claims directly to your insurance company as a courtesy to help streamline your reimbursement process. Payment is due at the time of service, and reimbursement (if any) is sent directly to you based on your plan’s coverage.
✔ Complimentary Insurance Verification
We offer free verification of your out-of-network benefits before your first visit so you know what to expect. Please note that benefit verification is not a guarantee of coverage or payment. Click Here for our verification form.
✔ FSA & HSA Payments Accepted
We accept Flexible Spending Accounts (FSA) and Health Savings Accounts (HSA) for all eligible services.
✔ For Your Records: CPT Codes We Commonly Use
If you prefer to call your insurer yourself, you can ask about out-of-network acupuncture benefits using the following commonly billed CPT codes:
99202 – New patient evaluation (approx. 20 min)
99203 – New patient evaluation (approx. 30 min)
97810 – Acupuncture, initial 15 min (no electrical stimulation)
97811 – Acupuncture, each additional 15 min (no electrical stimulation)
97813 – Acupuncture, initial 15 min (with electrical stimulation)
97814 – Acupuncture, each additional 15 min (with electrical stimulation)
20560 – Dry needling, 1–2 muscles
20561 – Dry needling, 3+ muscles
97140 – Manual therapy (e.g., myofascial release, trigger point therapy)
We do not follow up with insurance companies after claim submission, and we cannot guarantee reimbursement. However, we are happy to provide treatment notes or documentation upon request to support your claim if needed.
We do not participate with Medicare or Medicaid, including Part C out-of-network coverage. Medicaid Advantage may provide some reimbursement.
If you have secondary out-of-network coverage, this may be an option for reimbursement.
Yes, I offer a free phone-based Q&A session to see if we are the right fit to work together. This is an opportunity to address your questions and ensure that my approach aligns with your health goals. You may book your Q&A session here: Schedule an Appointment or Free Phone Consultation
Most people feel a quick muscle movement (that local twitch response we talked about), a brief cramp, or a dull ache. Some spots might be a bit more sensitive, but overall, it’s usually not too uncomfortable. Dr. Barber is very careful to make the effective treatment as beneficial as possible with minimal discomfort.
How many treatment sessions you’ll need depends on your specific problem, how long you’ve had it, and your general health. Some issues get better after just a few visits, but long-term or tricky conditions might need more treatment. Dr. Barber will talk with you about your personal treatment plan during your first visit. The effectiveness of dry needling can vary, but many find it an effective treatment for trigger point therapy.
When done by a trained expert like Dr. Barber, who is among the licensed acupuncturists also skilled in this Western medicine technique, dry needling is very safe. We always use clean, new needles for each patient and follow strict healthcare safety rules. Dr. Barber will ask about your health history to make sure it’s safe for you, especially if you take blood thinners or have a weakened immune system (compromised immune systems).
It’s a good idea to have eaten something before you come. Wear comfy, loose clothes so Dr. Barber can easily reach the area that needs treatment. And please, bring any questions you have about your condition or the dry needling treatment! Schedule an Appointment or Free Phone Consultation
Generally, no. For most people and most conditions, expertly performed dry needling is highly effective without ultrasound guidance. While ultrasound can be a helpful tool in rare, very specific situations, research suggests it doesn’t necessarily make dry needling treatment more effective for common trigger points.³ Dr. Barber relies on his extensive training, precise anatomical knowledge, and years of experience to deliver safe and effective treatment. Some clinics may push for routine ultrasound guidance, but this can often lead to unnecessary costs. For a more detailed explanation, you can read Dr. Barber’s article: Do You Need Ultrasound Guided Dry Needling?
Pelvic floor dry needling is a targeted treatment using thin filiform needles to release trigger points and muscle tension in the pelvic floor. It may help reduce pain, improve muscle function, and restore normal movement patterns.
Most patients feel a brief muscle twitch or cramp-like sensation during treatment. Discomfort is usually short-lived and often followed by a feeling of release or relief.
We maintain your comfort and privacy while working within your boundaries. Depending on the location being treated, undressing may be needed, but always with appropriate draping/covering. Internal examination and techniques are not performed or required.
Yes. I treat adults of all genders and identities. I provide a welcoming, inclusive environment. For post-operative gender-affirming care involving the pelvic floor, please bring surgical notes so we can assess appropriateness and safety together as each patient is very unique.
The number of treatments varies depending on the condition, its severity, and your response. Many patients notice improvement within 3–6 sessions, though complex cases may require longer-term care.
Yes, when performed by a trained, licensed provider with experience in pelvic anatomy. All needles are sterile and single-use. The procedure is precise and tailored to your needs and comfort level.
In NY State the only providers legally allowed to perform dry needling are Medical Doctors (MD), Doctors of Osteopathic Medicine (DO), Nurse Practitioners (NP), Physician Assistants (PA), and Acupuncturists (LAc). It is forbidden by the State Board for Chiropractors (DC) and Physical Therapists (PTs) to perform dry needling regardless of their training. For your safety, please choose a provider that is both properly trained and legally allowed to perform the technique.
Most pelvic floor conditions do benefit from dry needling, especially those involving muscle tension, trigger points, or nerve irritation. However, I require all pelvic floor patients to have an active diagnosis from a qualified medical provider or pelvic floor physical therapist. This is because dry needling is often just one part of the overall treatment strategy—it works best when integrated with a broader care plan that may include physical therapy, medical management, or other interventions. My goal is to ensure that dry needling is applied safely and appropriately as part of a comprehensive approach tailored to your specific diagnosis.