If you’re living with an overactive bladder, constant urinary frequency, sudden urgency, or urge incontinence, you already know how disruptive these symptoms can be. At our clinic, we offer Percutaneous Tibial Nerve Stimulation (PTNS) as a safe, non-surgical treatment option that targets the root of the problem without the side effects of medications or the risks of invasive procedures.

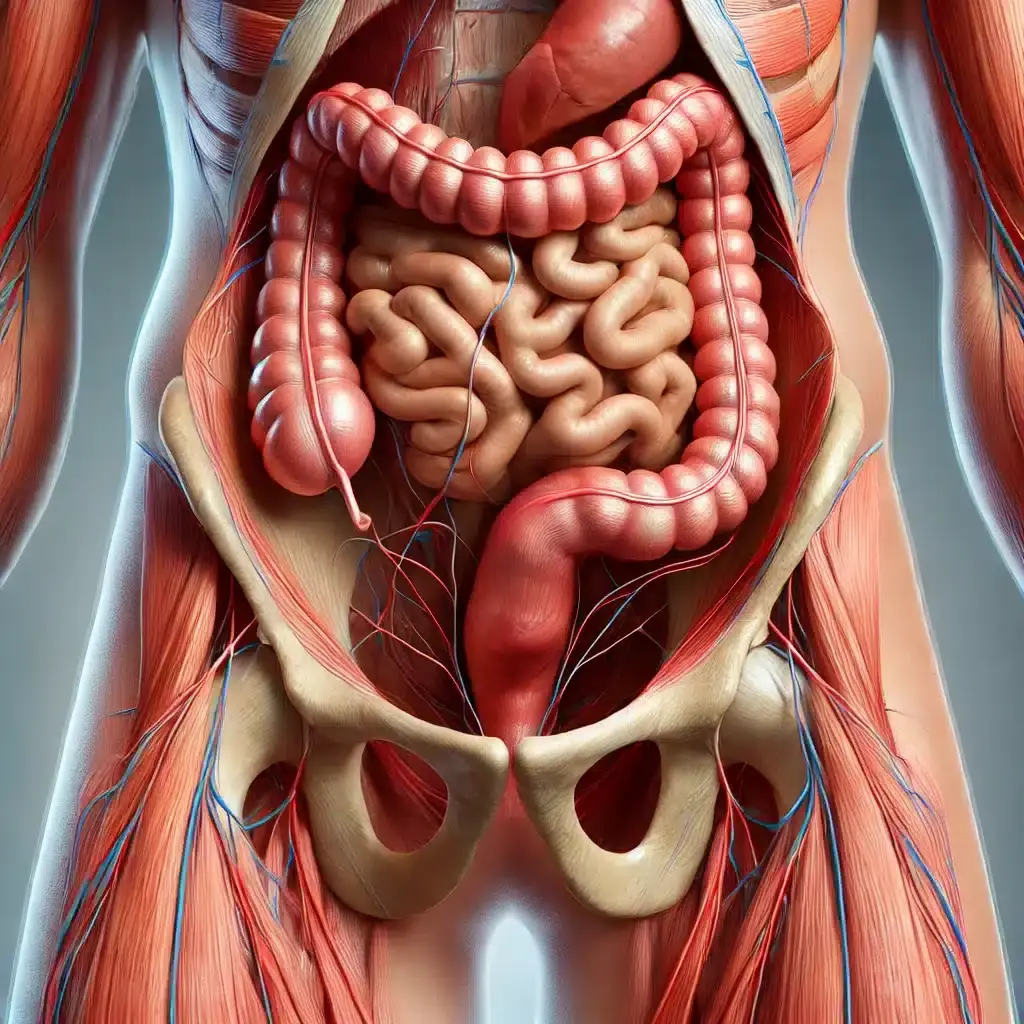
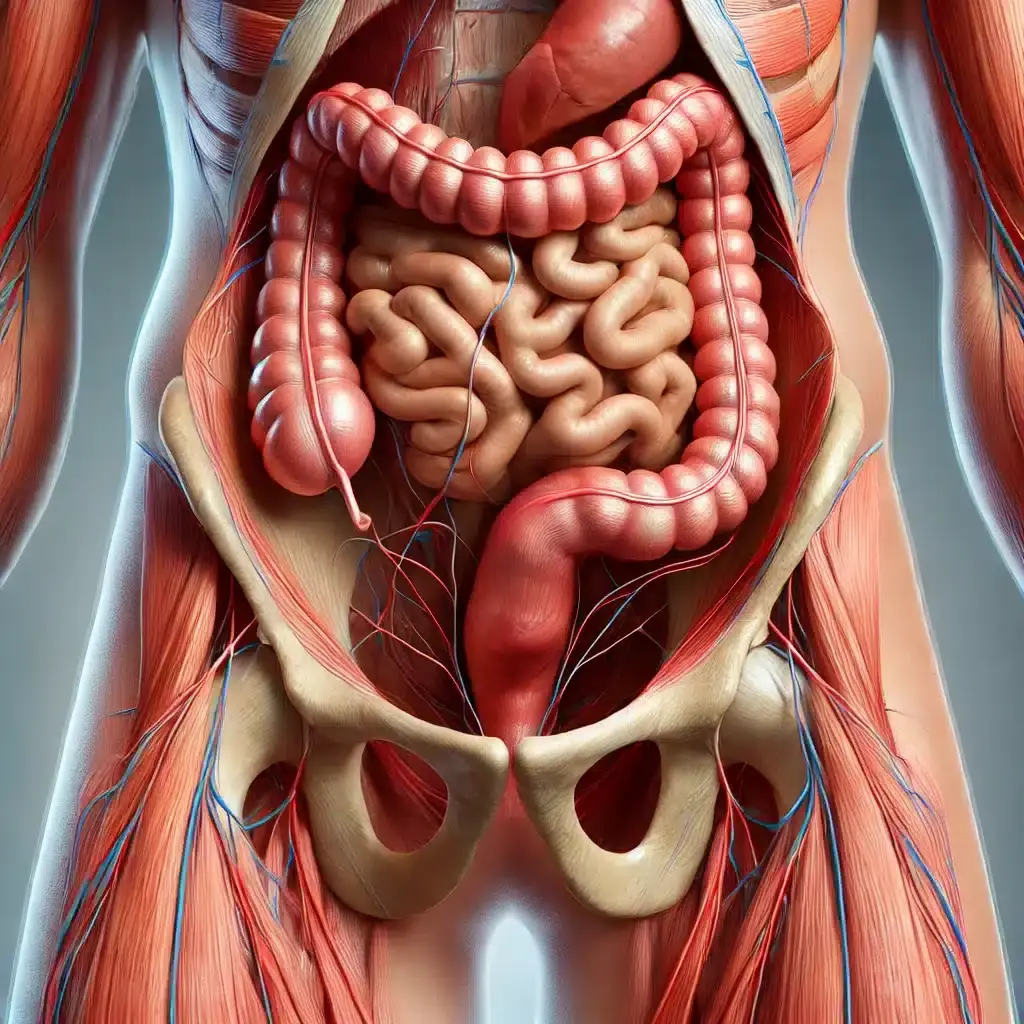
Percutaneous Tibial Nerve Stimulation (PTNS) is a neuromodulation therapy used to manage bladder dysfunction, particularly symptoms related to overactive bladder and urge incontinence. It involves placing a very fine needle electrode near the tibial nerve at the ankle. This nerve connects to the sacral plexus, the nerve center that controls bladder and pelvic floor function.
By sending mild electrical impulses through the tibial nerve, PTNS gently alters the signaling between your bladder and brain, helping to normalize urinary patterns over time.
The bladder is controlled by a complex system of nerves. When that system becomes overactive, it sends signals to empty the bladder too frequently—even when it’s not full. PTNS works by calming this hyperactive loop. The process:
Sessions last approximately 30 minutes, typically done weekly for 12 weeks. Many patients begin to notice symptom improvement within the first few weeks.
Most people describe PTNS as a tingling or pulsing sensation in the ankle or foot. It is relatively painless, and no anesthesia or downtime is required. After each session, you can return to your normal activities immediately.
Yes. PTNS is FDA-approved for treating overactive bladder and is backed by high-quality research. Studies show it to be a safe, well-tolerated, and effective therapy, even compared to medication:
As a specialist in pelvic floor dysfunction, I offer PTNS not as a standalone procedure, but as part of a comprehensive, personalized treatment plan. Here’s what sets our clinic apart:
By combining PTNS with these pelvic floor therapies, we often see faster, more profound results with improved symptom durability.
You may be a good candidate if you:
Patients with neurological conditions, post-surgical pelvic pain, or postpartum dysfunction may also benefit when PTNS is integrated into a larger pelvic rehabilitation strategy.
If you’ve been searching for a safe, noninvasive solution for overactive bladder, urinary urgency, urinary frequency, or urge incontinence, PTNS may be the answer. Combined with targeted pelvic floor therapies like dry needling and acupuncture, it offers a powerful, patient-centered path to lasting relief.
Schedule your PTNS consultation today and let’s create a plan that helps you move forward—confidently and comfortably.