When men hear the term “pelvic floor,” the common reaction is often one of dismissal—a belief that it is a topic relevant only to women, particularly concerning pregnancy and childbirth. This pervasive misconception has created a silent health crisis, leaving millions of men to struggle with debilitating symptoms they don’t understand and are often too embarrassed to discuss. The reality, however, is that the male pelvic floor is a critical anatomical structure, fundamental to core stability, bladder and bowel control, and sexual function. When it malfunctions, the impact on a man’s quality of life can be profound.
This report delves into the often-overlooked world of men’s pelvic health, moving beyond anecdotal evidence to present a clear, data-driven picture of the issues at hand. By examining robust statistics from academic and clinical research, it aims to dismantle the stigma and shed light on the prevalence of conditions like chronic pelvic pain, urinary incontinence, and erectile dysfunction. The numbers are not just surprising; they are a call to action, revealing that these problems are far more common than most men believe and, most importantly, that effective, evidence-based solutions exist.
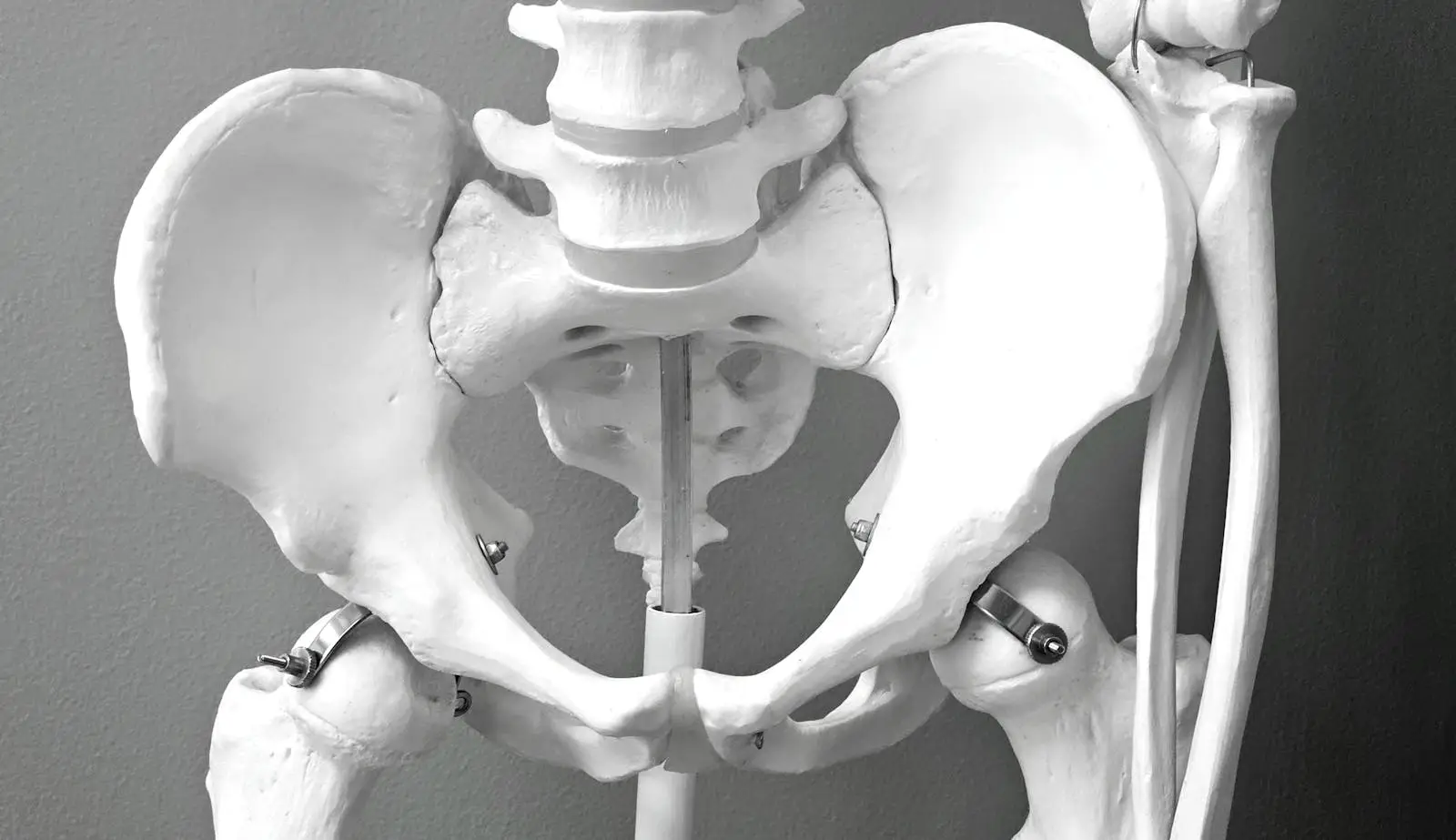
Before exploring the statistics of dysfunction, it is essential to understand the structure and function of the male pelvic floor. It is not an isolated muscle but a sophisticated and integral part of the body’s core system.
Imagine a strong, flexible hammock or sling made of muscles, ligaments, and connective tissues stretching from the pubic bone at the front of the pelvis to the tailbone (coccyx) at the back.1 This is the pelvic floor. This muscular base forms the bottom of the pelvic bowl, providing support for the organs contained within it.1 The primary muscles that make up this structure are the levator ani and the coccygeus, which work together to form a dynamic and supportive floor.3
Crucially, the pelvic floor does not operate in isolation. It is a key component of the body’s “core,” a group of muscles that includes the diaphragm (the main breathing muscle), the deep abdominal muscles, and the back muscles.4 This integrated system works together to stabilize the spine and pelvis, manage pressure within the abdomen, and facilitate movement. The pelvic floor is also highly interconnected with the muscles of the hips and glutes, meaning that its function can be influenced by posture, gait, and overall musculoskeletal health.3This intricate network is controlled by a complex web of nerves that allow for both voluntary control (like consciously squeezing the muscles) and involuntary, automatic function.3
The male pelvic floor performs three essential roles that are fundamental to daily life and well-being. Understanding these functions is key to appreciating the significant impact of pelvic floor dysfunction.
The interconnected nature of the pelvic floor means that a problem in one area can have cascading effects. For instance, because the pelvic floor is part of the core and works with the diaphragm, dysfunctional breathing patterns or poor posture can alter the pressure management system in the torso, placing undue strain on the pelvic floor muscles. This demonstrates that pelvic floor health is not just about a single group of muscles but is intrinsically linked to the function of the entire body. A problem manifesting as pelvic pain might not originate in the pelvis itself but could be a symptom of a broader musculoskeletal or neuromuscular imbalance. This holistic view is critical for understanding and effectively treating pelvic floor dysfunction.
The statistics surrounding male pelvic floor dysfunction are compelling and reveal a landscape of common but under-recognized health issues. The data provides a powerful argument for bringing this topic out of the shadows and into mainstream health conversations.
For decades, persistent pelvic pain in men was almost universally attributed to an issue with the prostate gland and labeled “chronic prostatitis.” However, an overwhelming body of evidence now shows that this diagnosis is often incorrect and that the problem lies within the complex neuromuscular structures of the pelvic floor itself.
The prevalence of what is more accurately termed Chronic Pelvic Pain Syndrome (CP/CPPS) is startling. Worldwide, it is estimated to affect between 2% and 16% of men.9 A large, nationally representative study in Australia provided an even clearer picture, finding that nearly
one in six men (18%) reported experiencing some form of pelvic pain within the past year.11 This makes CP/CPPS the single most common urological diagnosis in men under the age of 50.10
The most critical statistic in this area reveals a profound gap in medical diagnosis: while these symptoms are often presumed to be caused by a prostate infection, research shows that in 90% to 95% of cases, no bacterial pathogen can be identified.12 This means that for the vast majority of men suffering from chronic pelvic pain, antibiotics and other prostate-focused treatments are unlikely to be effective because they do not address the true root of the problem.
Furthermore, the condition is not just a physical one. Research has uncovered a strong and consistent link between chronic pelvic pain and mental health. Men with pelvic pain are significantly more likely to have a history of anxiety or depression.11 One study found that men with CP/CPPS were more than 2.5 times as likely as controls to suffer from a mental illness, with a particularly high frequency of anxiety and panic disorders.13 Another study found that a history of physical, emotional, or sexual abuse was associated with a 1.7 to 3.3 times higher likelihood of having CP/CPPS.13
This collection of evidence points to an unavoidable conclusion: chronic pelvic pain in men is rarely a simple infection. It is a complex condition that requires a biopsychosocial approach to treatment. The lack of infection in most cases, combined with the strong correlation with psychological distress, indicates that the condition involves more than just the pelvic tissues. It involves the central nervous system, which can become “sensitized” or wound-up, amplifying pain signals from the pelvic region. This process, known as central sensitization, means the brain and spinal cord become overprotective, interpreting normal sensations as painful.13 This explains why stress and anxiety can worsen symptoms. Therefore, effective treatment cannot be one-dimensional. It must be interdisciplinary, combining pelvic floor physical therapy to address muscle tension and dysfunction, pain medicine to help calm the overactive nervous system, and psychological support to manage the anxiety, stress, and trauma that often fuel the pain cycle.13
Urinary incontinence (UI), the involuntary leakage of urine, is another condition often mistakenly associated primarily with women. However, statistics show it is a significant and growing problem for men, with profound implications for both individual well-being and public health.
A comprehensive analysis of US national health data revealed an alarming trend: the overall prevalence of any UI among men rose from 11.5% in the 2001-2002 period to 19.3% by 2017-2020.14 This means that today, nearly
one in five men in the United States experiences some form of urinary leakage.
While UI can affect men at any stage of life, the risk increases substantially with age. Studies show that the prevalence climbs to between 21% and 32% in elderly men.15 One large survey found that while 11% of men aged 60-64 experienced incontinence, that figure rose to 31% for men aged 85 and older.16
Importantly, male UI is not just an isolated bladder issue; it is closely linked to a range of other health conditions. Research has identified significant associations between UI and factors such as a high body mass index (BMI), smoking, physical inactivity, depression, and hypertension.14 The presence of other chronic diseases like diabetes and a history of stroke are also major risk factors.15
The strong correlation between urinary incontinence and these major chronic diseases suggests that UI in men should be viewed as more than a simple “plumbing problem.” It can serve as a bellwether for an individual’s overall health status. The risk factors for UI—obesity, inactivity, hypertension, diabetes—are the very same risk factors for cardiovascular disease and metabolic syndrome. The rising prevalence of male UI is likely occurring in tandem with these other epidemics of lifestyle-related disease. This reframes UI from a mere urological symptom to a potential public health indicator. It also has significant economic consequences; the presence of UI more than doubles a person’s annual medical expenditures.18 This understanding implies that a powerful strategy for preventing or mitigating UI in men involves addressing these root causes. Interventions focused on improving diet, increasing physical activity, and managing weight could have a dual benefit, improving not only bladder control but also overall cardiovascular and metabolic health.
For men diagnosed with localized prostate cancer, radical prostatectomy—the surgical removal of the prostate gland—is a common and often life-saving treatment. However, it carries a significant risk of side effects that can severely impact quality of life, with urinary incontinence being one of the most feared.
The reported prevalence of post-prostatectomy incontinence (PPI) varies wildly in the literature, with figures ranging from as low as 1% to as high as 87%.19 This confusingly wide range is due to inconsistencies in how studies define “incontinence” (e.g., one drop of leakage vs. needing multiple pads per day), the timing of assessment after surgery, and the specific surgical technique used.19
To get a clearer, more realistic sense of the long-term impact, it is helpful to look at large, community-based studies with extended follow-up. One such study found that 14% of men still reported frequent urinary leakage or no urinary control five years after their surgery.20 This statistic underscores that for a substantial minority of men, PPI is not a temporary issue that resolves within a few months but a persistent, long-term challenge.
The reason for this high risk lies in anatomy. The prostate gland surrounds the urethra, and both the prostate itself and the internal urethral sphincter at the base of the bladder contribute to urinary control.21 During a radical prostatectomy, these structures are removed. Post-operative continence, therefore, becomes almost entirely dependent on the health and function of the external urethral sphincter (also known as the rhabdosphincter) and the surrounding pelvic floor muscles.19 The nerves that control this sphincter are located in very close proximity to the prostate and are highly susceptible to being stretched or damaged during the procedure.5
Furthermore, urinary incontinence is not the only potential continence issue. A rarely discussed complication is fecal incontinence. One study that surveyed men after radical prostatectomy found that fecal incontinence occurred in 5% of those who had a retropubic (abdominal) approach and a striking 18% of those who had a perineal approach. Perhaps most concerning was the finding that the majority of these men had never reported the problem to their doctor, highlighting the profound stigma associated with this symptom.22
Given that post-surgical continence relies so heavily on the remaining sphincter and pelvic floor muscles, the importance of pre- and post-operative rehabilitation cannot be overstated. Since the surgery inherently compromises one part of the continence system, optimizing the function of the remaining parts is paramount. This points to the critical role of “prehabilitation”—seeing a pelvic floor physical therapist before surgery. A therapist can teach a man how to properly isolate, strengthen, and control his pelvic floor muscles, ensuring they are in the best possible condition to take over the work of maintaining continence after the procedure. Studies have shown that poor preoperative muscle function is a significant predictor of persistent incontinence.21 Therefore, the conversation around prostate cancer treatment should expand beyond just cancer cure rates to include a robust discussion of functional preservation. Proactively engaging in pelvic floor rehabilitation before and after surgery could be one of the most effective strategies for mitigating one of the treatment’s most distressing side effects.
Erectile dysfunction (ED) is a common condition that significantly affects men’s self-esteem and relationships. While often linked to cardiovascular health, hormones, or psychological factors, a crucial mechanical component is frequently overlooked: the pelvic floor.
The scope of the problem is vast. It is estimated that ED affects approximately 10% of otherwise healthy men. This rate climbs dramatically in the presence of other health conditions, affecting 28% of men with diabetes and 39% of men with heart disease.8 The public narrative around treatment is dominated by pharmacological solutions like sildenafil. However, a growing body of evidence shows that for many men, the solution may lie in a targeted exercise program.
The pelvic floor muscles are not passive bystanders in sexual function; they are active participants. Specifically, the ischiocavernosus and bulbospongiosus muscles have a direct mechanical role in producing and maintaining an erection. When a man is aroused, these muscles contract, which increases the pressure within the penis and compresses the veins that drain blood away. This action traps blood within the erectile tissues, leading to a firm and sustained erection.8 Weakness or poor coordination of these muscles can therefore directly contribute to the inability to achieve or maintain an erection.
This mechanical link is the basis for one of the most hopeful and empowering statistics in men’s health. A landmark randomized controlled trial—the gold standard of clinical research—investigated the effect of a structured program of pelvic floor muscle exercises on men with ED. The results were remarkable: the exercise program restored normal erectile function in 40% of the participants. An additional 35.5% of men saw significant improvement in their erectile function.8 In total, over 75% of the men in the study benefited from the therapy.
This evidence provides a compelling argument for a paradigm shift in how ED is treated. While medication can be effective at managing symptoms, it does not address the underlying cause for men whose ED stems from pelvic floor weakness. Pelvic floor muscle training, on the other hand, targets a potential root cause of the problem. This makes it an evidence-based, primary intervention, not an “alternative” therapy. Pelvic floor physical therapy should be presented to men as a first-line treatment option, either alongside or even before medication is considered. It offers the prospect of a long-term resolution without the potential side effects, ongoing costs, and dependency associated with pharmacological treatments. This is a profoundly empowering message that offers a proactive, non-drug path to recovery for a significant portion of men suffering from ED.
The data on men’s pelvic floor dysfunction can be extensive. The following table provides a clear, scannable summary of the most critical statistics discussed in this report, highlighting the prevalence of these common conditions and the significance of the findings.
| Condition | Key Statistic | Significance | Primary Source(s) |
| Chronic Pelvic Pain | Affects up to 16% of menglobally; often misdiagnosed. | A common, misunderstood condition, especially in men under 50. | Dydyk AM, et al. 2025 9; Smith CP. 2016 10 |
| General Urinary Incontinence | Prevalence in US men rose to 19.3% by 2020. | A widespread and growing public health issue linked to lifestyle. | Cao C, et al. 2022 14 |
| Age-Related Incontinence | Affects up to 31% of men aged 85 and older. | Demonstrates a significant increase in risk with advanced age. | Anger JT, et al. 2006 16 |
| Post-Prostatectomy Incontinence | 14% of men report frequent leakage 5 years after surgery. | Highlights the significant long-term risk to quality of life. | Penson DF, et al. 2005 20 |
| Erectile Dysfunction & PFMT | 40% regained normal function with pelvic floor exercises. | Proves that a non-drug intervention can resolve a root cause of ED. | Dorey G, et al. 2004 8; 2005 23 |
Understanding the statistics is the first step. The next is taking action. Improving pelvic floor health is possible, but it begins with correctly identifying the muscles and understanding that the right approach depends on the specific problem.
Before you can exercise a muscle, you must be able to feel it working. The pelvic floor muscles can be subtle, but there are a few safe and effective ways to identify them.2
One of the most critical concepts in pelvic floor health is that “Kegels are not always the answer.” Pelvic floor dysfunction can stem from muscles that are too weak (hypotonic) or muscles that are too tight and overactive (hypertonic). The treatment for these two problems is completely different.
Because it is impossible to know whether your muscles are weak or tight without a proper assessment, it is essential to seek professional guidance. A pelvic floor therapist is a healthcare professional specially trained to evaluate the function of these muscles. They can determine the underlying issue and design a safe and effective treatment plan tailored to your specific needs.
Once the basic contraction is mastered, more specific cues can be used to target different functions. To focus on the front part of the pelvic floor, which is important for urinary continence and erectile function, the cue “try to shorten your penis” can be effective. To target the back part, which is crucial for bowel control, the cue “tighten the muscle around your anus” is more direct.5
Lifestyle factors also play a significant role. For men with CP/CPPS, some find that their symptoms are aggravated by certain foods and beverages. One study found that spicy foods, coffee, hot peppers, and alcoholic beverages were the most common triggers.10 Conversely, regular, moderate physical activity, such as brisk walking, has been associated with a significantly lower risk of developing CP/CPPS.10
The evidence is clear and compelling: pelvic floor dysfunction is a common, statistically significant, and deeply impactful health issue for men. From the chronic pain that disrupts the lives of younger men to the incontinence that can accompany aging or cancer treatment, and the erectile dysfunction that affects men of all ages, these conditions are not rare abnormalities. They are widespread problems that have been shrouded in silence and stigma for too long.
Yet, the most important message to emerge from the data is one of hope. These conditions are not an inevitable part of aging or an untreatable life sentence. Robust scientific evidence demonstrates that effective, targeted treatments exist. The finding that a structured exercise program can restore normal erectile function in 40% of men is a powerful testament to the body’s capacity for healing.8 The understanding that most chronic pelvic pain is not an incurable infection but a treatable neuromuscular condition opens the door to relief for millions.13
This knowledge must now translate into action. It is time to discard the outdated notion that the pelvic floor is not a man’s concern. It is time to break the silence that prevents men from seeking help, as evidenced by the fact that most men with post-prostatectomy fecal incontinence never tell their doctor.22 If you are experiencing any of the symptoms discussed in this report—pain, leakage, or sexual dysfunction—it is essential to speak with a healthcare provider or a pelvic floor therapist. Taking that first step is not a sign of weakness; it is a sign of strength and a commitment to reclaiming your health and quality of life.