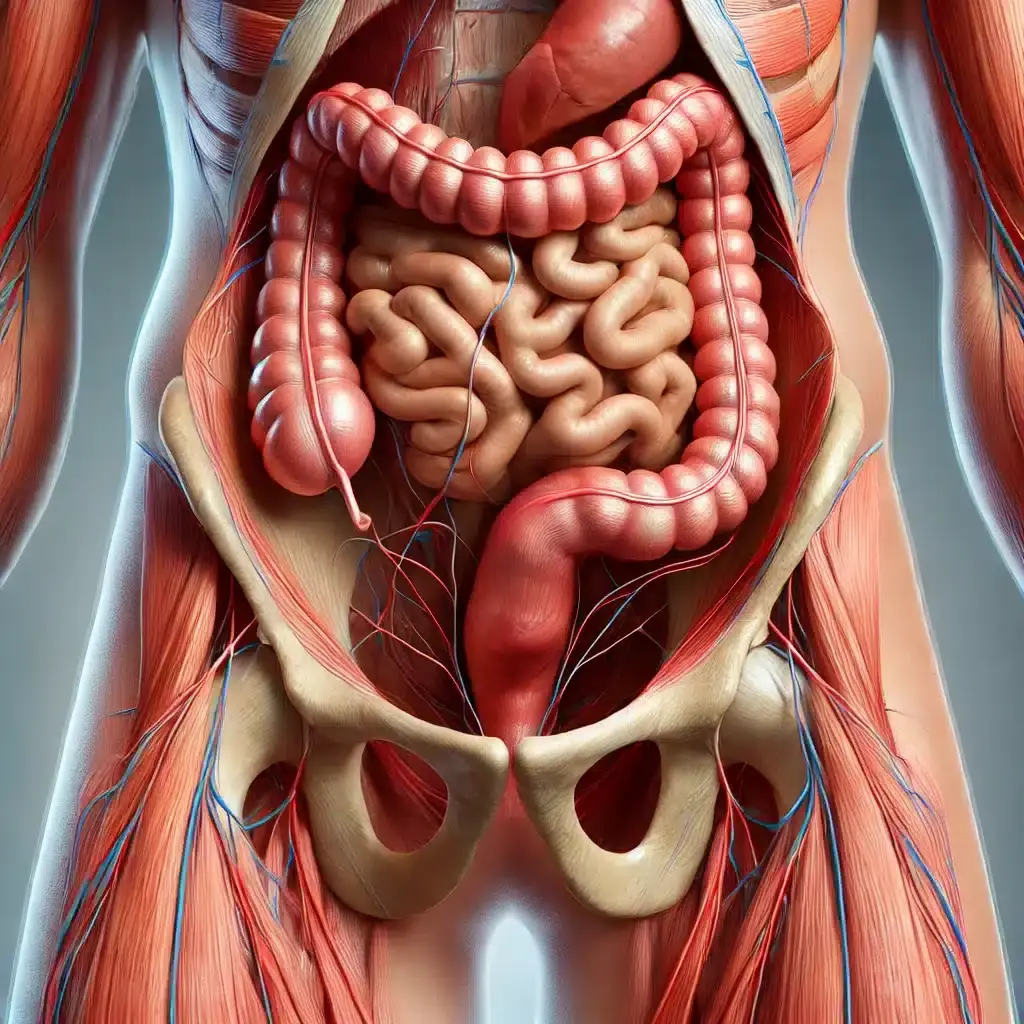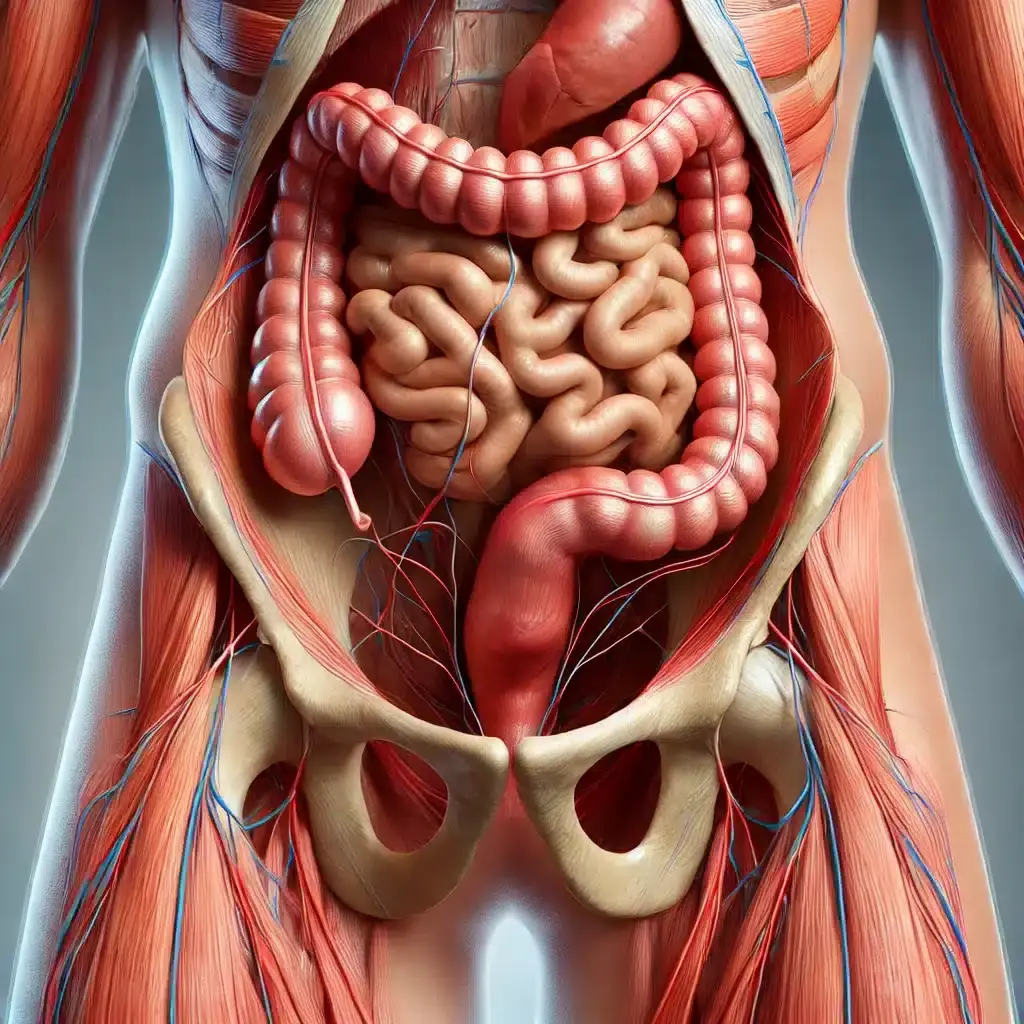
Endometriosis is a chronic disease affecting many young women of reproductive age, characterized by severe pain, painful periods, heavy menstrual bleeding, and painful intercourse. Endometriosis occurs when endometrial cells, which normally line the uterus, grow outside the uterus, typically within the pelvic cavity, affecting pelvic organs such as fallopian tubes, ovaries, rectovaginal septum, and uterosacral ligaments. Common endometriosis symptoms include abdominal pain, lower back pain, menstrual periods with intense cramps, and issues during sexual intercourse.

Several factors may increase the risk of developing endometriosis. These include family history of endometriosis, short menstrual cycles, early age at first menstrual period, and conditions such as pelvic inflammatory disease. Additionally, factors like retrograde menstruation—a condition where menstrual blood containing endometrial cells flows back through the fallopian tubes into the pelvic cavity—increase risk. Research indicates a higher risk of endometriosis among women with reproductive health conditions like ovarian cysts, ovarian cancer, and irritable bowel syndrome.¹
The most common symptom of endometriosis is chronic pain, particularly severe during menstrual periods. Other signs include heavy menstrual bleeding, painful menstrual cramps, abdominal pain, lower back pain, pain during sexual intercourse, and gastrointestinal discomfort resembling irritable bowel syndrome. Women may also experience infertility, known as endometriosis-associated infertility, and emotional stress affecting mental health.²
Endometriosis often leads to pelvic floor dysfunction, marked by tight or uncoordinated pelvic floor muscles. These muscular issues significantly contribute to chronic pain, impacting both reproductive and mental health. A 2023 clinical trial by Fernández-Peña et al. showed that pelvic floor physiotherapy (PFP), including Thiele massage (gentle stretching and digital pressure), effectively reduced pelvic tension, pain, and discomfort.³
A 2019 case report by Morin et al. demonstrated that physical therapy helped eliminate chronic pain in a woman with severe stage IV endometriosis after surgery.⁴
Dry needling targets painful areas known as trigger points within pelvic floor muscles and addresses scar tissue resulting from previous laparoscopic surgery—a common treatment for endometriosis. Scar tissue can cause additional pain and complications. According to a 2020 report by Anderson et al., dry needling involves inserting thin needles into these trigger points and areas of scar tissue, reducing muscle tension, softening scar tissue, and disrupting pain signals.⁵
Acupuncture, widely recognized for pain management, has proven effective for managing endometriosis pain. A 2018 systematic review by Zhu et al. found acupuncture significantly reduces pelvic pain among women suffering from endometriosis.⁶ Acupuncture works by reducing inflammation and regulating pain signals, offering long-term relief.
Definitive diagnosis of endometriosis typically requires laparoscopic surgery, a surgical procedure where healthcare providers examine and remove endometriosis lesions through small cuts in the abdomen. However, healthcare professionals may initially use pelvic exams, transvaginal ultrasounds, or magnetic resonance imaging (MRI) to detect ovarian cysts or deeper endometriosis involvement. Endometriosis stages range from superficial endometriosis to deep endometriosis and ovarian endometriomas.
Common medical therapies include hormonal contraceptives (birth control pills), Gonadotropin-releasing hormone (GnRH) agonists, nonsteroidal anti-inflammatory drugs (NSAIDs), and pain medications. However, these treatments can have side effects, such as bone loss, and might not address all symptoms. Consequently, integrating alternative treatments like acupuncture and pelvic floor dry needling can enhance care and outcomes without significant adverse effects.
Given endometriosis’ complexity, combining acupuncture, pelvic floor physiotherapy, and dry needling may offer the most effective treatment. This multimodal strategy addresses symptoms from multiple angles, managing chronic pain, enhancing reproductive health, and improving quality of life while managing and minimizing side effects.
My Upper West Side, NYC clinic specializes in these integrative approaches, providing personalized care tailored to your symptoms and needs and I work with your existing care team. To learn more or schedule an appointment, contact my office today.