Understanding the complex interplay between our body’s systems can be a fascinating journey. Especially when it comes to seemingly unrelated conditions like constipation and hip pain.
Does constipation cause hip pain? It’s a question that might seem odd at first. However, the answer is more intricate than you might think.
Research indicates that approximately 12% of men and 16% of women suffer from constipation.1
In this article, we delve into the physiological and anatomical links between constipation and hip pain. We’ll explore how the pressure and discomfort from constipation can manifest as hip pain.
We’ll also discuss the broader implications of constipation on the body’s musculoskeletal system. This includes the potential for constipation to cause perineal pain and discomfort in the groin area.
By the end, you’ll have a comprehensive understanding of this topic. This will help you make informed decisions about your health or provide valuable insights to your readers.
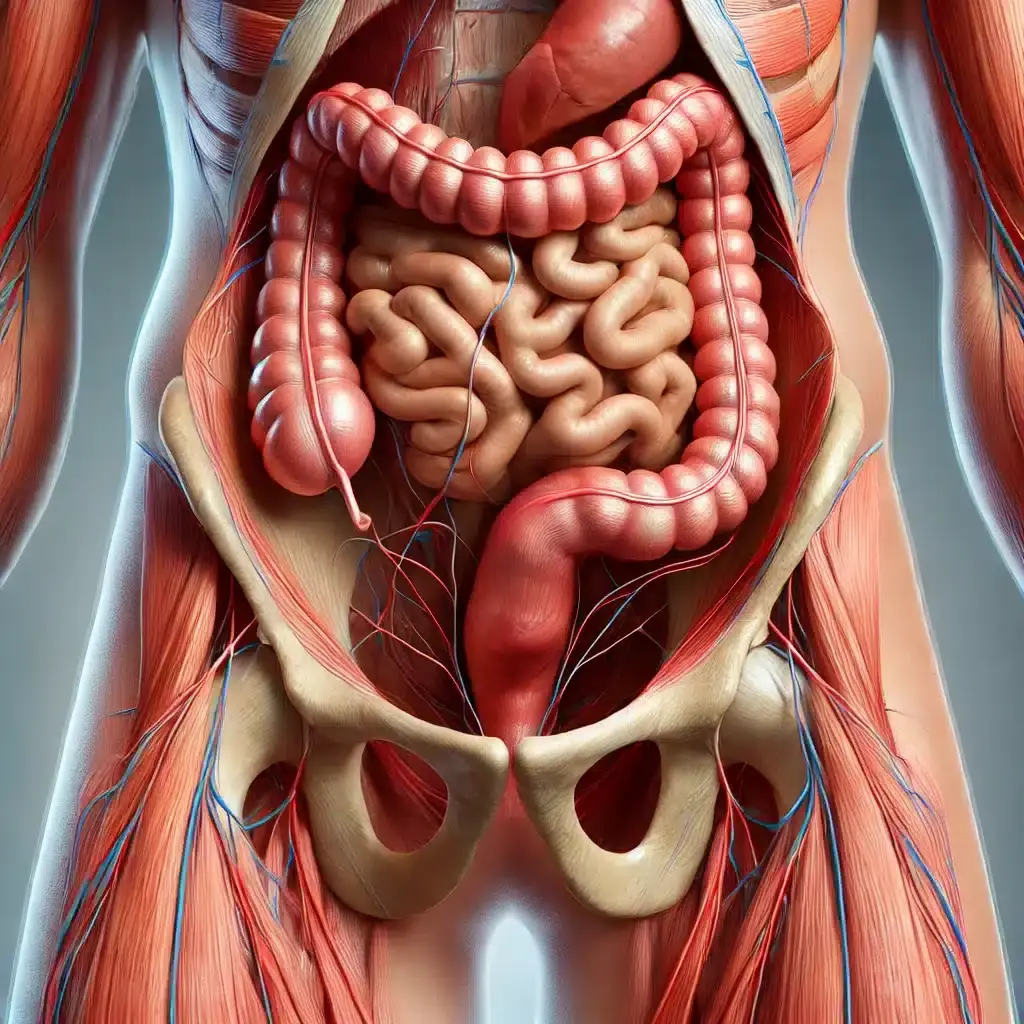
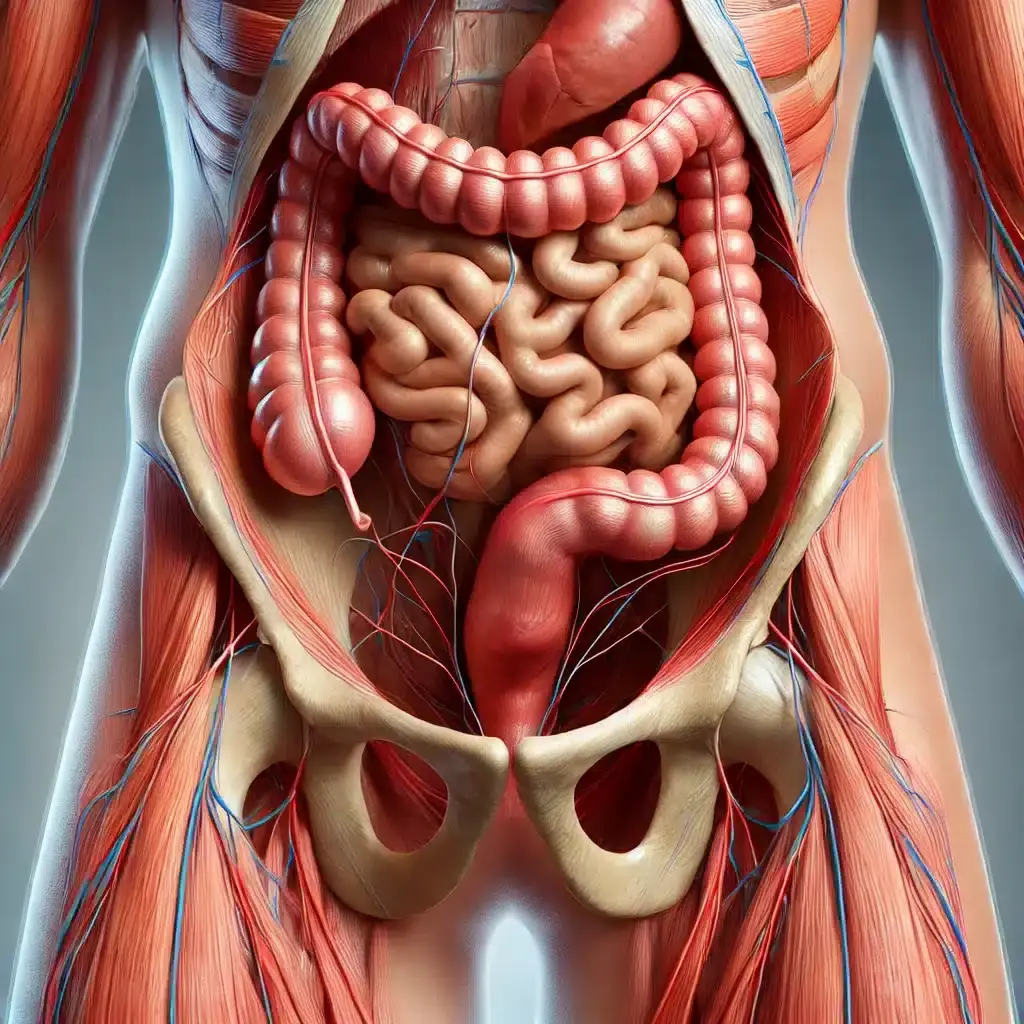
The large intestine plays a significant role in the body and is closely situated to the hip structures. This anatomical proximity means that any issues in the intestine, such as constipation, can directly impact the hip area.
So can constipation cause hip pain? Referred pain is a common phenomenon where discomfort is felt in an area away from the actual source of pain. With constipation, the increased pressure in the abdomen can lead to this referred pain in the hips. It’s a unique relationship that can easily be overlooked.
Can constipation cause perineal pain? The psoas muscle, a key player located near both the hips and the intestines, often becomes tense due to constipation. This tension can further exacerbate pain in the hip. Understanding this muscle’s role highlights how bowel health can influence musculoskeletal well-being.
Moreover, the pelvic floor muscles, which also sit near these structures, can be strained by bowel irregularities. This strain can result in discomfort or even pain extending to the hips. It is crucial to consider these anatomical connections when addressing constipation-related pain.
This intricate interplay between these structures underlines the importance of viewing the body holistically. By understanding these connections, holistic health approaches can target relief effectively.
Can constipation cause pain in the groin? Constipation can manifest in surprising ways, including hip pain. This connection may not be immediately obvious but is important to recognize. Identifying symptoms early can lead to more effective management.
Many individuals experience discomfort that extends beyond the abdomen due to constipation. The pressure from constipation often radiates, causing pain in adjacent areas like the hips. Awareness of these symptoms helps guide appropriate care.
Common symptoms of constipation-related hip pain include:
In addition to hip pain, individuals may also feel discomfort in the perineum or groin. This is due to shared nerve pathways that carry signals from these regions. Constipation can stress these pathways, leading to broad areas of pain.
Groin pain and perineal pain may coexist with hip pain, complicating diagnosis. It is important to consider constipation as a potential underlying cause. Recognizing these patterns can be essential for those seeking relief through holistic health approaches. Understanding the interconnectedness of symptoms can lead to more comprehensive treatment strategies.
Traditional Chinese Medicine (TCM) offers a unique viewpoint on constipation and hip pain. TCM focuses on treating the body as an integrated whole. This approach aims to restore balance and harmony to the body’s systems.
Acupuncture is a key component of TCM. It has been used for centuries to address various ailments, including pain. Practitioners believe that acupuncture can relieve constipation and associated pains, like those in the hip.
Central to TCM is the concept of Qi stagnation. Qi, or energy, must flow smoothly throughout the body. When Qi becomes blocked, it can lead to discomfort and pain, including in the hip region.
The mind-gut connection further illustrates this holistic view. Modern research supports the idea that gut health affects overall well-being. Stress and emotions can disrupt gut function, which may manifest as physical pain.
This link shows how important it is to pay attention to emotional health.
Relaxation techniques can reduce stress, aiding in constipation relief. By calming the mind, you may also alleviate physical symptoms.
Holistic approaches encourage viewing the body as a cohesive system. Understanding the links between mind, gut, and musculoskeletal health is crucial. This integrative perspective helps individuals manage and reduce constipation-related hip pain effectively.
Diet plays a key role in preventing constipation and associated hip pain. Incorporating the right foods can promote digestive health and reduce discomfort.
Key dietary changes include:
Hydration is equally important in managing constipation. Water aids in moving food through the digestive tract. Aim to drink adequate fluids daily, as dehydration can worsen symptoms.
Regular exercise is another crucial factor. Physical activity helps stimulate bowel movements and relieve constipation. Aim for at least 30 minutes of moderate exercise most days of the week.
Stress management techniques should not be overlooked. Stress can contribute to both constipation and musculoskeletal pain. Adopting relaxation techniques can help.
Consider activities such as yoga and meditation. These practices promote relaxation and improved digestion. They also encourage mindfulness, which can aid in recognizing and managing stress triggers.
Implementing these lifestyle changes can have a significant impact. An integrative approach supports better digestive and musculoskeletal health.
Beyond immediate relief, long-term habits sustain digestive wellness. Consistency in diet, hydration, and exercise helps maintain regular bowel movements, reducing pain risks.
Pelvic floor dry needling is an innovative technique that can provide significant relief for individuals experiencing hip pain and related constipation issues. This method involves the insertion of thin needles into specific trigger points within the pelvic floor muscles, promoting relaxation and reducing tension. By targeting these areas, dry needling can help alleviate discomfort and improve overall pelvic health.
The pelvic floor consists of a group of muscles that support the bladder, bowel, and uterus. When these muscles become tight or dysfunctional, they can contribute to pain in the hips and lower abdomen, as well as exacerbate constipation. Dry needling helps to release muscle tension, improve blood flow, and enhance the body’s natural healing processes.
Medications like laxatives can provide quick relief for constipation. However, they should be used cautiously. Over-reliance on laxatives may lead to dependency, weakening natural bowel function over time.
There are many types of laxatives. It’s essential to choose the right one for the situation. Consulting a healthcare provider is advisable to avoid potential side effects and ensure safety.
Probiotics offer a promising alternative for managing constipation. These beneficial bacteria support gut health and improve bowel regularity. They work by enhancing the microbial balance within the digestive system, promoting efficient digestion.
Including probiotics in the diet can be straightforward. They are found in fermented foods like yogurt and kefir. Probiotic supplements are also widely available and can be an effective addition to one’s regimen. The consistent use of probiotics may lead to long-term improvements in digestive health and related discomfort, including hip pain.
Regular bowel movements are crucial for overall health. They help prevent the accumulation of waste and pressure in the abdomen. Maintaining regularity supports the musculoskeletal system and reduces the risk of hip pain.
Building a strong core can aid in managing constipation-related discomfort. Core strengthening exercises promote better posture. This can help alleviate pressure on the hips and spine.
Pelvic alignment exercises are also beneficial. These exercises focus on maintaining proper posture and balance. Proper alignment can reduce the strain on muscles connected to the hip area.
Sleep quality plays a vital role in digestive and musculoskeletal health. Poor sleep can disrupt bowel function and exacerbate pain. Prioritizing restful sleep can improve overall well-being.
A balanced diet is another key component. Consuming a diet rich in fiber helps promote regular bowel movements. Adequate hydration supports digestive processes and may help relieve tension in the hips.
To incorporate these measures:
Commitment to these habits can lead to long-term improvements in digestion and hip health. Regular medical check-ups can aid in monitoring progress. They also help in adjusting strategies when needed.
A holistic approach offers a comprehensive path to wellness. Integrating diet, lifestyle changes, and alternative therapies can effectively address constipation and associated hip pain. This multifaceted strategy provides a more balanced and thorough solution.
Personalized treatment plans are vital for managing symptoms. Each individual’s health profile is unique, necessitating tailored approaches. Consulting with healthcare professionals ensures the most effective strategies are employed.
Continued research is essential to deepen our understanding of the connection between constipation and hip pain. Educating both patients and practitioners enhances outcomes. Promoting awareness and knowledge can lead to improved health and quality of life.
If you are struggling with hip pain and constipation, consider exploring pelvic floor dry needling as part of your treatment plan. Our experienced practitioners are here to help you find the relief you deserve.
Book an appointment today to discuss how pelvic floor dry needling can benefit your condition and enhance your overall well-being. Don’t let discomfort hold you back—take action towards a healthier, pain-free life!
References:
1 Pinto Sanchez MI, Bercik P. Epidemiology and burden of chronic constipation. Can J Gastroenterol. 2011;25(Suppl B):11B–15B. doi:10.1155/2011/974573.