Deep pelvic or perineal aching
Often worse with prolonged sitting, cycling, or after a long workday, and may feel “internal” rather than on the skin.
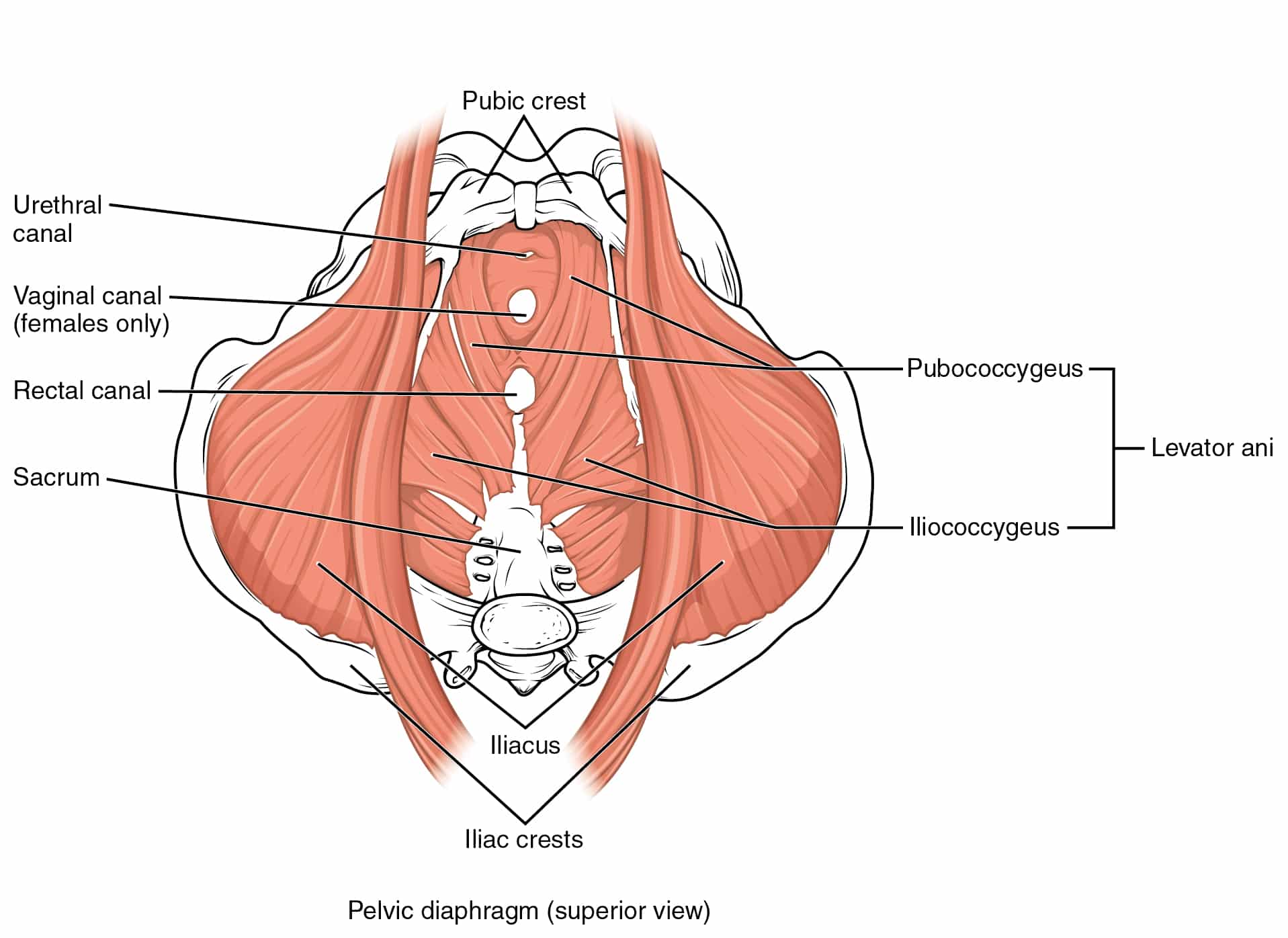
Pelvic Myofascial Pain Syndrome is often less about a single “injured structure” and more about a protective myofascial pattern that develops across the pelvic floor, hips, adductors, abdominal wall, and low back. Irritable trigger points can refer pain into the perineum, groin, tailbone, lower abdomen, or genitals, and can also create non-pain symptoms such as urinary urgency or bowel discomfort through guarding and altered coordination.
Over time, the nervous system can become sensitized. That means even after the initial driver settles, the area remains reactive, with muscles that tighten quickly, reduced tissue glide, and a lower threshold for flare-ups. The clinical task is to identify the specific referral map and movement positions that reproduce symptoms, then reduce the myofascial and neural drivers while rebuilding tolerance to sitting, loading, and daily function.
This care is complementary to pelvic floor physical therapy and medical evaluation. We focus on functional drivers that can coexist with, or persist after, medically managed conditions.
Standard care often splits pelvic pain into either “structural” (seen on imaging) or “chemical” (treated with medications). Myofascial pain and trigger point referral patterns frequently do not show up on MRI or ultrasound, and medications can reduce symptoms without changing tissue sensitivity, guarding, or coordination.
When treatment is not guided by palpation findings and symptom mapping, the root driver can be missed. Generic stretching can aggravate an already guarded pelvic floor. Core strengthening without controlling hip and adductor tone can increase compression and trigger point activity. If sensitization is part of the picture, purely local treatment without a phased capacity plan can lead to short-lived gains.
Not necessarily. Those are medical diagnoses managed by medical providers. Myofascial pain can coexist with them or persist after they are treated. Our role is to evaluate functional drivers such as trigger point referral, guarding, and nerve interface irritability, and to coordinate care when medical evaluation is needed.
Imaging can be important for ruling in or out structural pathology, but it often does not identify trigger points or guarding patterns. We use hands-on palpation, symptom reproduction, referral mapping, and movement testing to determine which tissues and positions are driving your symptoms.
When appropriate and with explicit consent, pelvic floor assessment and treatment can include internal palpation and pelvic floor dry needling. External-only approaches are also available and can be effective depending on the driver. We discuss options and choose the least invasive path that matches your presentation.
Most patients start with 1 to 2 visits per week for a short period to reduce reactivity and clarify drivers, then taper as capacity improves. Your plan is based on irritability level, duration of symptoms, and the demands of your work and training schedule.
Yes, temporary soreness or a short flare can happen, especially with sensitization. We manage this by precise dosing, conservative tissue selection early on, and pairing treatment with positioning and activity guidance. The goal is meaningful improvement in function and predictability, not aggressive provocation.
Seek urgent medical care for fever, chills, unexplained bleeding, new urinary retention, severe escalating pain, saddle anesthesia, progressive leg weakness, or any concern for infection or other acute medical issues. We coordinate referrals when symptoms fall outside a functional myofascial pattern.
While acupuncture does not hurt, you may feel a “de qi” sensation—a deep, dull ache or heaviness at the point of insertion when the thin needles stimulate the connective tissue and nervous system. This is a natural and effective part of the acupuncture treatment, indicating that the acupuncture point is being activated. The patient is always in control, and most find these sensations well-tolerated or enjoyable. Schedule an Appointment or Free Phone Consultation
Most people feel a quick twitch or brief pinch during a dry needling session as the needle interacts with myofascial trigger points or muscle fibers in the affected area, but it’s usually well tolerated and any muscle soreness fades quickly—many patients say the relief is worth it. Schedule an Appointment or Free Phone Consultation
The benefits of dry needling are numerous, especially for pain management. This treatment method effectively targets myofascial trigger points within tight muscles, helping to release muscle tension, improve muscle function and range of motion, and stimulate the body’s natural healing process. It can be particularly effective for soft tissue injuries, overuse injuries, and chronic pain conditions like myofascial pain syndrome by addressing the root causes of discomfort in specific areas of the body. Many find it helps accelerate recovery time from a muscle strain or injury. Schedule an Appointment or Free Phone Consultation
This varies based on the patient’s medical history and condition, but many patients see results over time depending on their condition. Pain-related conditions often initially have quick results, though recovery time can differ. This will be discussed during the initial consultation. Schedule an Appointment or Free Phone Consultation
Yes, acupuncture and dry needling complement most standard medical treatments, including physical therapy treatments or chiropractic care, and Dr. Barber can collaborate with other healthcare providers as needed. Schedule an Appointment or Free Phone Consultation
The first acupuncture appointment or dry needling session includes a detailed initial consultation where Dr. Barber reviews the medical history, discusses specific needs and musculoskeletal condition, performs an assessment, and provides the first personalized treatment option. Schedule an Appointment or Free Phone Consultation
Yes, I treat adults, teens, and children (though I do not specialize in infants or toddlers). I’m experienced in working with sensitive issues and strive to create a welcoming, inclusive space for all patients, including those in the LGBTQIA+ community. For pelvic floor patients who are post-operative following gender-affirming surgery, I do not have specialized training in this area, but if you’re able to provide detailed surgical notes, I’m open to collaborating and finding safe, supportive treatment solutions together. Schedule an Appointment or Free Phone Consultation
Yes — we are an out-of-network provider and can submit to most PPO insurance plans. While we are not contracted with any insurance companies, we want to make it as easy as possible for you to use your benefits when available.
We do not participate with Medicare or Medicaid, including Part C out-of-network coverage.
✔ Claims Submitted on Your Behalf
We now submit out-of-network claims directly to your insurance company as a courtesy to help streamline your reimbursement process. Payment is due at the time of service, and reimbursement (if any) is sent directly to you based on your plan’s coverage.
✔ Complimentary Insurance Verification
We offer free verification of your out-of-network benefits before your first visit so you know what to expect. Please note that benefit verification is not a guarantee of coverage or payment. Click Here for our verification form.
✔ FSA & HSA Payments Accepted
We accept Flexible Spending Accounts (FSA) and Health Savings Accounts (HSA) for all eligible services.
✔ For Your Records: CPT Codes We Commonly Use
If you prefer to call your insurer yourself, you can ask about out-of-network acupuncture benefits using the following commonly billed CPT codes:
99202 – New patient evaluation (approx. 20 min)
99203 – New patient evaluation (approx. 30 min)
97810 – Acupuncture, initial 15 min (no electrical stimulation)
97811 – Acupuncture, each additional 15 min (no electrical stimulation)
97813 – Acupuncture, initial 15 min (with electrical stimulation)
97814 – Acupuncture, each additional 15 min (with electrical stimulation)
20560 – Dry needling, 1–2 muscles
20561 – Dry needling, 3+ muscles
97140 – Manual therapy (e.g., myofascial release, trigger point therapy)
We do not follow up with insurance companies after claim submission, and we cannot guarantee reimbursement. However, we are happy to provide treatment notes or documentation upon request to support your claim if needed.
We do not participate with Medicare or Medicaid, including Part C out-of-network coverage. Medicaid Advantage may provide some reimbursement.
If you have secondary out-of-network coverage, this may be an option for reimbursement.
Yes, I offer a free phone-based Q&A session to see if we are the right fit to work together. This is an opportunity to address your questions and ensure that my approach aligns with your health goals. You may book your Q&A session here: Schedule an Appointment or Free Phone Consultation
Most people feel a quick muscle movement (that local twitch response we talked about), a brief cramp, or a dull ache. Some spots might be a bit more sensitive, but overall, it’s usually not too uncomfortable. Dr. Barber is very careful to make the effective treatment as beneficial as possible with minimal discomfort.
How many treatment sessions you’ll need depends on your specific problem, how long you’ve had it, and your general health. Some issues get better after just a few visits, but long-term or tricky conditions might need more treatment. Dr. Barber will talk with you about your personal treatment plan during your first visit. The effectiveness of dry needling can vary, but many find it an effective treatment for trigger point therapy.
When done by a trained expert like Dr. Barber, who is among the licensed acupuncturists also skilled in this Western medicine technique, dry needling is very safe. We always use clean, new needles for each patient and follow strict healthcare safety rules. Dr. Barber will ask about your health history to make sure it’s safe for you, especially if you take blood thinners or have a weakened immune system (compromised immune systems).
It’s a good idea to have eaten something before you come. Wear comfy, loose clothes so Dr. Barber can easily reach the area that needs treatment. And please, bring any questions you have about your condition or the dry needling treatment! Schedule an Appointment or Free Phone Consultation
Generally, no. For most people and most conditions, expertly performed dry needling is highly effective without ultrasound guidance. While ultrasound can be a helpful tool in rare, very specific situations, research suggests it doesn’t necessarily make dry needling treatment more effective for common trigger points.³ Dr. Barber relies on his extensive training, precise anatomical knowledge, and years of experience to deliver safe and effective treatment. Some clinics may push for routine ultrasound guidance, but this can often lead to unnecessary costs. For a more detailed explanation, you can read Dr. Barber’s article: Do You Need Ultrasound Guided Dry Needling?
Pelvic floor dry needling is a targeted treatment using thin filiform needles to release trigger points and muscle tension in the pelvic floor. It may help reduce pain, improve muscle function, and restore normal movement patterns.
Most patients feel a brief muscle twitch or cramp-like sensation during treatment. Discomfort is usually short-lived and often followed by a feeling of release or relief.
We maintain your comfort and privacy while working within your boundaries. Depending on the location being treated, undressing may be needed, but always with appropriate draping/covering. Internal examination and techniques are not performed or required.
Yes. I treat adults of all genders and identities. I provide a welcoming, inclusive environment. For post-operative gender-affirming care involving the pelvic floor, please bring surgical notes so we can assess appropriateness and safety together as each patient is very unique.
The number of treatments varies depending on the condition, its severity, and your response. Many patients notice improvement within 3–6 sessions, though complex cases may require longer-term care.
Yes, when performed by a trained, licensed provider with experience in pelvic anatomy. All needles are sterile and single-use. The procedure is precise and tailored to your needs and comfort level.
In NY State the only providers legally allowed to perform dry needling are Medical Doctors (MD), Doctors of Osteopathic Medicine (DO), Nurse Practitioners (NP), Physician Assistants (PA), and Acupuncturists (LAc). It is forbidden by the State Board for Chiropractors (DC) and Physical Therapists (PTs) to perform dry needling regardless of their training. For your safety, please choose a provider that is both properly trained and legally allowed to perform the technique.
Most pelvic floor conditions do benefit from dry needling, especially those involving muscle tension, trigger points, or nerve irritation. However, I require all pelvic floor patients to have an active diagnosis from a qualified medical provider or pelvic floor physical therapist. This is because dry needling is often just one part of the overall treatment strategy—it works best when integrated with a broader care plan that may include physical therapy, medical management, or other interventions. My goal is to ensure that dry needling is applied safely and appropriately as part of a comprehensive approach tailored to your specific diagnosis.