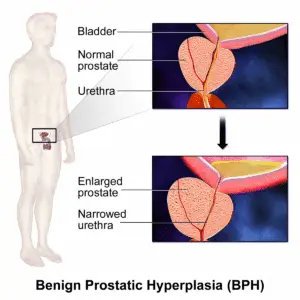
Benign Prostatic Hyperplasia (BPH)—or enlarged prostate—is a common condition that affects nearly half of all men over age 50, and up to 90% by age 80.¹ While BPH is not cancerous, it often causes urinary urgency, frequency, weak stream, and incomplete emptying. What’s less commonly addressed is how these symptoms can lead to—or be aggravated by—pelvic floor dysfunction.
At my clinic, I offer pelvic floor dry needling as a part of an integrative approach for men with chronic pelvic discomfort, urinary symptoms, or postural tension stemming from prostate-related issues. Whether you’ve been diagnosed with BPH or are simply living with unexplained pelvic pressure and urinary symptoms, dry needling may help address the muscular patterns that are often overlooked.
BPH is the non-cancerous enlargement of the prostate gland. As the prostate grows, it can compress the urethra and irritate the bladder, leading to lower urinary tract symptoms (LUTS) such as:
These symptoms are typically treated with medications (like alpha-blockers or 5-alpha-reductase inhibitors) or procedures that reduce prostate size. However, many patients continue to experience pelvic discomfort, urinary tension, or pain, even after medical treatment.
Men with BPH often develop compensatory tension in the pelvic floor muscles. When urination becomes difficult or incomplete, the body recruits nearby musculature—especially the levator ani, obturator internus, bulbospongiosus, and urogenital diaphragm—to assist with bladder function.
Over time, this compensation can lead to:
Pelvic floor dry needling uses sterile, thin needles to target hypertonic or dysfunctional pelvic muscles, releasing trigger points and improving blood flow and tissue mobility. In the context of BPH-related symptoms, dry needling may:
Dry needling can be especially beneficial when combined with breath training, postural correction, and pelvic floor physical therapy.
A study in the Journal of Urology found that men with chronic pelvic pain syndrome felt better after getting myofascial physical therapy, which included trigger point release. More than half of the men in the study reported less pain and better urinary symptoms, showing this kind of hands-on treatment may help with pelvic floor muscle tension.1
BPH prevalence increases with age and commonly leads to LUTS.
Pelvic floor muscle training (PFMT) improves urinary symptoms in men with BPH.
Dry needling and myofascial therapy reduce pelvic pain and improve symptoms in men with pelvic floor dysfunction.
As a provider trained in pelvic floor dry needling and acupuncture, I take a neuromuscular approach to chronic pelvic symptoms. For men with BPH or post-prostate issues, care may include:
The goal is to normalize pelvic tone, improve urinary mechanics, and reduce pain and muscular guarding—not just manage symptoms.
If you’re dealing with urinary issues, pelvic tension, or lingering pain from BPH or related diagnoses, help is available. Dry needling and integrative pelvic care can address the muscular and fascial dysfunctions that medications often miss.
Conveniently located in NYC and specializing in male pelvic floor dysfunction and chronic pain.
Book your in-office consultation today and start reclaiming your comfort and control.