Shin splints, also known as medial tibial stress syndrome, are a common overuse injury that causes pain along the front of the lower leg. Often associated with high-impact activities like running and military training, shin splints can disrupt your routine and lead to persistent discomfort if left untreated. Understanding the causes, symptoms, and prevention methods is essential for maintaining an active lifestyle.
Whether you’re a young athlete, a military recruit, or someone who enjoys regular physical activity, the risk of shin splints increases with repetitive stress on the shinbone and surrounding muscles. Fortunately, with the right treatment options and preventive measures, you can effectively manage this condition and stay on track with your fitness goals.

Shin splints refer to pain along the front of the lower leg, medically termed medial tibial stress syndrome. This condition occurs when repetitive stress on the shinbone and surrounding muscles leads to inflammation of the muscles and connective tissues. Common among individuals engaged in high-impact activities, shin splints are particularly prevalent in runners and those undergoing military training (Newman et al., 2013; Menéndez et al., 2020).
Shin splints are one of the most common overuse injuries, especially in sports that involve high-impact exercises (Menéndez et al., 2020). They can also develop due to a sudden increase in physical activity or changes in a training program, making it crucial to carefully monitor activity levels. The condition is not limited to seasoned athletes; young athletes and beginners are also at risk, especially if proper techniques or equipment are neglected.
Several factors increase the likelihood of developing shin splints. Individuals with flat feet or rigid arches are at higher risk because their foot structure may not provide sufficient shock absorption during physical activity. Similarly, muscle imbalances, weak core muscles, or tight calf muscles can contribute to the condition by placing extra strain on the lower extremity (Newman et al., 2013; Menéndez et al., 2020). Wearing worn-out shoes or those lacking proper arch support further exacerbates the problem, as does running on uneven or hard surfaces that amplify repetitive stress on the lower leg.
Another significant risk factor is a sudden change in activity level, such as increasing running mileage too quickly or starting a more intense training program without adequate preparation. This is particularly common among military recruits or individuals participating in military training. Engaging in high-impact activities without proper conditioning or cross-training can also elevate the risk of shin splints (Saad et al., 2025).
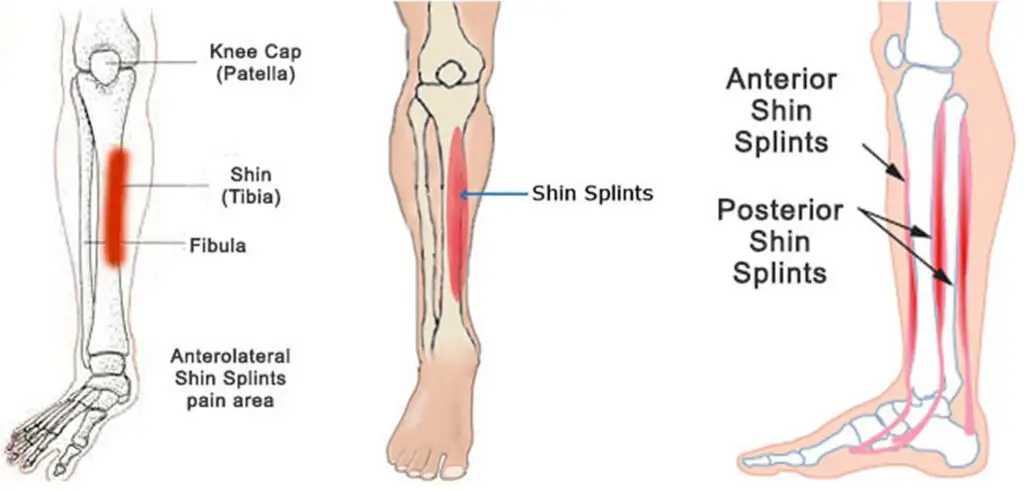
Shin splint symptoms typically include pain along the inner edge or front of your lower leg, often worsening during high-impact activities like running or jumping. The pain of shin splints can range from mild discomfort to severe shin pain that interferes with daily activities. Inflammation of the muscles and connective tissues around the shinbone is common, leading to noticeable tenderness or swelling in the affected area. Persistent lower leg pain during or after exercise may also indicate stress injuries, such as a stress reaction or stress fracture, which require immediate attention (Menéndez et al., 2020; Saad et al., 2025).
If shin pain persists or worsens despite self-care, it is essential to consult a health care professional. A medical history review and physical exam can help identify underlying issues such as stress reaction, compartment syndrome, or other medical conditions. In some cases, imaging tests like a bone scan or magnetic resonance imaging may be recommended to rule out more severe stress injuries. Sports medicine specialists or orthopedic surgeons can provide valuable guidance on how to treat shin splints effectively. The American Academy of Orthopedic Surgeons emphasizes the importance of seeking professional help for persistent symptoms to prevent complications and ensure a safe return to physical activity.
Dry needling is a therapeutic technique that targets muscle imbalances and inflammation, offering relief for individuals suffering from shin splints. Performed by skilled acupuncturists the procedure involves inserting thin needles into trigger points or knots in the muscles to promote healing and relaxation. Research has shown that dry needling of the soleus muscle in athletes with medial tibial stress syndrome can significantly reduce pain and improve function (Singh et al., 2025; Dogra & Singh, 2024).
This treatment is particularly effective for addressing anterior shin splints and running injuries, which often stem from repetitive stress and improper biomechanics. By reducing tension in the lower extremity and encouraging blood flow to the affected area, dry needling helps accelerate recovery and restore mobility.
Many patients choose dry needling for its ability to relieve shin splint symptoms and improve overall flexibility. It is especially beneficial for athletes, as it addresses underlying muscle imbalances that contribute to running injuries and stress injuries (Singh et al., 2025; Dogra & Singh, 2024). Beyond immediate symptom relief, dry needling supports long-term recovery by promoting healing in the bone tissue and lower leg muscles. It can be combined with other treatment options, such as physical therapy and strength training, to ensure a well-rounded approach to managing shin pain and preventing recurrence.
Self-care plays a crucial role in treating shin splints, especially in the early stages. Resting and gradually returning to physical activity can help alleviate symptoms and prevent further injury. Applying a cold pack to the affected area reduces inflammation, while supportive shoes and shock-absorbing insoles provide additional arch support during recovery. Low-impact exercises like swimming or cycling are excellent alternatives to high-impact activities, allowing you to maintain fitness without exacerbating shin pain (Menéndez et al., 2020; Marques et al., 2025).
Pain relievers such as nonsteroidal anti-inflammatory drugs can also help manage the pain of shin splints. Stretching exercises and strength training for the core and calf muscles can further support recovery and prevent future overuse injuries (Marques et al., 2025).
In some cases, medical treatments may be necessary to treat shin splints effectively. Physical therapy can help address muscle imbalances and improve flexibility, while imaging tests may be needed to assess the extent of stress injuries. A detailed medical history and physical exam can provide additional insights into the root cause of shin pain and guide treatment decisions. Professional organizations like the American Academy of Orthopaedic Surgeons offer resources to help patients navigate recovery and prevent complications.
Preventing shin splints begins with proper preparation and attention to your physical activity routine. Wearing proper running shoes with adequate arch support is essential, particularly for individuals with flat feet, high arches, or rigid arches (Newman et al., 2013; Menéndez et al., 2020). Supportive shoes and shock-absorbing insoles reduce the impact on your lower leg muscles and shinbone, minimizing the repetitive stress that leads to shin pain (Marques et al., 2025). Additionally, replacing worn-out shoes regularly ensures optimal support during high-impact activities.
Incorporating strength training and stretching exercises into your fitness routine can address muscle imbalances and improve flexibility in the calf and core muscles. Gradually increasing your activity level and avoiding sudden changes in intensity or mileage are also critical in preventing overuse injuries (Marques et al., 2025; Saad et al., 2025). Low-impact exercises like swimming or cycling can be excellent alternatives to high-impact activities, providing a way to maintain fitness without placing undue stress on the lower extremity.
Cross-training and running on softer or more even surfaces can further reduce the strain on your lower leg. For those recovering from shin splints, a well-structured training program under the guidance of a physical therapist or sports medicine specialist can help you safely return to activity while minimizing the risk of recurrence (Marques et al., 2025). Preventing shin splints not only protects your lower leg muscles and connective tissues but also ensures you can continue enjoying physical activity in the long term.
If you are dealing with shin splints or want to prevent them altogether, expert care is available in NYC. Book a dry needling appointment at our Upper West Side clinic to begin your personalized treatment plan. Dr. Barber, experienced in sports medicine is dedicated to helping you recover and achieve your fitness goals.
Do not let shin pain disrupt your active lifestyle. With professional guidance, effective treatment options, and preventive strategies, you can stay on track and maintain a healthy, pain-free routine. Contact us today to start your recovery journey.
Dogra, H., & Singh, P. (2024). Investigating the effect of dry needling on myofascial trigger point in soleus muscle of soccer players with medial tibial stress syndrome. Journal of Modern Rehabilitation, 18(4), 421–426. http://dx.doi.org/10.18502/jmr.v18i4.16910
Marques, T. B. T., et al. (2025). Preventive interventions for medial tibial stress syndrome. Gait & Posture.https://www.sciencedirect.com/science/article/abs/pii/S0966636225005685
Menéndez, C., Calvo-Maseda, A., et al. (2020). Medial tibial stress syndrome in novice and recreational runners: A systematic review. International Journal of Environmental Research and Public Health, 17(20), 7457. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7663311/
Newman, P., Witchalls, J., Waddington, G., & Adams, R. (2013). Risk factors associated with medial tibial stress syndrome in runners: A systematic review. Open Access Journal of Sports Medicine, 4, 229–241. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3873798/
Saad, M. A., et al. (2025). Medial tibial stress syndrome: A scoping review of epidemiology, biomechanics, and risk factors. Cureus. https://www.cureus.com/articles/345672-medial-tibial-stress-syndrome-a-scoping-review-of-epidemiology-biomechanics-and-risk-factors
Singh, A., Wadhwani, N., & Sharma, M. (2025). Short-term effectiveness of dry needling on pain and ankle range of motion in athletes with medial tibial stress syndrome: A randomized controlled trial. Journal of Manual & Manipulative Therapy, 33(1), 47–53. https://pubmed.ncbi.nlm.nih.gov/39097941/