Jaw muscle pain, especially in the masseter, can make jaw movement, chewing, and even smiling difficult. This powerful skeletal muscle plays a crucial role in elevating the lower jaw and closing the bite, but when it develops muscle spasms, trigger points, or tension, it often results in TMJ pain and related pain conditions.
Understanding the common causes, symptoms, and treatment options for masseter dysfunction can help patients and healthcare providers work together toward the most appropriate treatment plan—one that restores comfortable jaw function and reduces muscle tension.
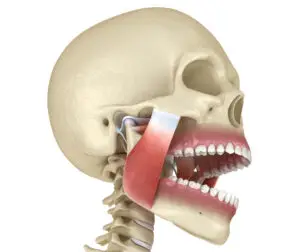
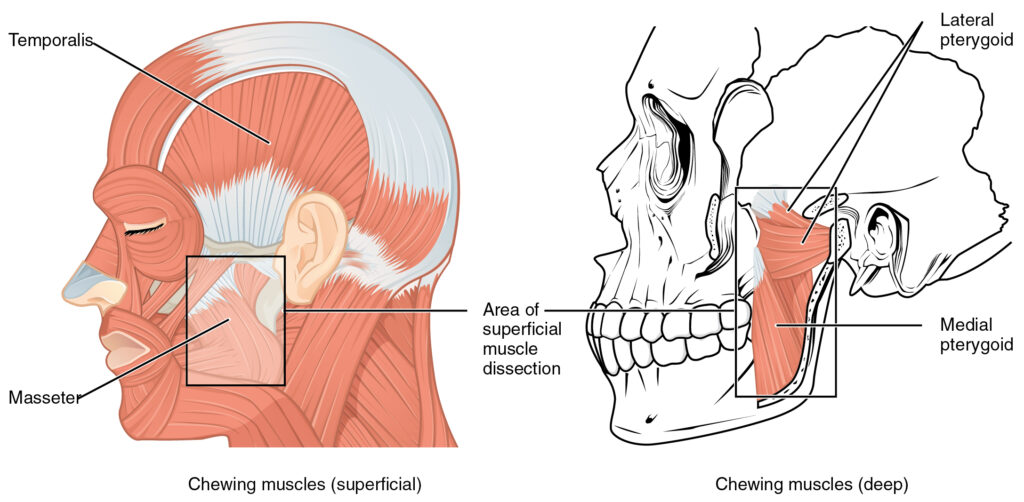
The masseter is often called the strongest muscle in the human body relative to size. It has a superficial layer, the superficial masseter muscle, and a deep masseter portion, attaching from the zygomatic arch to the jaw bone. This jaw muscle works in coordination with the temporalis muscle, lateral pterygoid muscle, and other facial muscles to power chewing. Together, they are innervated by branches of the trigeminal nerve.
When muscle fibers tighten due to emotional stress, jaw clenching, or posture problems, the result can be jaw tension, tension-type headache, and difficulty keeping the mouth open. In more advanced cases, this can lead to temporomandibular joint disorders or temporomandibular joint syndrome.
Common symptoms of masseter dysfunction include
Trigger points are small, hypersensitive nodules within the soft tissue of the masseter that lower the pressure pain threshold and reproduce acute pain when pressed. Studies using a rating scale in clinical trials show how these points often refer discomfort to
Trigger points in the deep masseter may cause severe pain, while the superficial layer can spread discomfort to broader areas of the jaw and face.
Simple jaw exercises and jaw relaxation strategies can provide effective treatment at home.
When self-care isn’t enough, a healthcare provider or physical therapist may recommend advanced treatment options such as
For patients with underlying medical conditions like Rheumatoid Arthritis or Neuropathic Pain, care may require a multidisciplinary team.
If you’re living with jaw tension, tension headaches, or jaw muscle pain that interferes with eating or speaking, the right treatment plan can make all the difference. At Dr. Jordan Barber Clinic in NYC, we specialize in orthopedic dry needling and acupuncture for TMJ pain, masseter dysfunction, and pain management.
Our integrative approach provides the best experience by addressing both the common cause of symptoms and the surrounding neck muscles and facial muscles that perpetuate dysfunction. Whether you’re struggling with acute pain or chronic temporomandibular joint disorders, we create customized treatment options for long-term relief.
Biel, A., & Dorn, R. (2010). Trail guide to the body: A hands-on guide to locating muscles, bones and more. Books of Discovery.
Corcoran, N. M., & Goldman, E. M. (2024). Anatomy, head and neck, masseter muscle. In StatPearls. StatPearls Publishing. Treasure Island (FL). https://www.ncbi.nlm.nih.gov/books/NBK539869/
Fernández-Carnero, J., La Touche, R., Ortega-Santiago, R., Galan-del-Rio, F., Pesquera, J., Ge, H. Y., & Fernández-de-Las-Peñas, C. (2010). Short-term effects of dry needling of active myofascial trigger points in the masseter muscle in patients with temporomandibular disorders. Journal of Orofacial Pain, 24(1), 106–112. https://pubmed.ncbi.nlm.nih.gov/20213033/
Janda, V. (1983). Muscle function testing. Butterworth-Heinemann.
Mierzwa, D., Olchowy, C., Olchowy, A., Nawrot-Hadzik, I., Dąbrowski, P., Chobotow, S., Grzech-Leśniak, K., Kubasiewicz-Ross, P., & Dominiak, M. (2022). Botox therapy for hypertrophy of the masseter muscle causes a compensatory increase of stiffness of other muscles of the masticatory apparatus. Life, 12(6), 840. https://doi.org/10.3390/life12060840
Shen, Y. F., & Goddard, G. (2007). The short-term effects of acupuncture on myofascial pain patients after clenching. Pain Practice, 7(3), 256–264. https://doi.org/10.1111/j.1533-2500.2007.00140.x
Travell, J. G., & Simons, D. G. (1993). Myofascial pain and dysfunction: The trigger point manual. Lippincott Williams & Wilkins.
Witmanowski, H., & Błochowiak, K. (2020). The whole truth about botulinum toxin: A review. Advances in Dermatology and Allergology, 37(6), 853–861. https://doi.org/10.5114/ada.2019.82795